Chapter: Medical Surgical Nursing: Musculoskeletal Care Modalities
Managing the Patient With an External Fixator
Managing
the Patient With an External Fixator
External fixators are
used to manage open fractures with soft tis-sue damage. They provide stable
support for severe comminuted (crushed or splintered) fractures while
permitting active treat-ment of damaged soft tissues (Fig. 67-2). Complicated
fractures of the humerus, forearm, femur, tibia, and pelvis are managed with
external skeletal fixators. The fracture is reduced, aligned, and immobilized
by a series of pins inserted in the bone. Pin po-sition is maintained through
attachment to a portable frame. The fixator facilitates patient comfort, early
mobility, and active exer-cise of adjacent uninvolved joints. Complications
related to dis-use and immobility are minimized.
Nursing Interventions
It is important to prepare the patient psychologically
for applica-tion of the external fixator. The apparatus looks clumsy and
for-eign. Reassurance that the discomfort associated with the device is minimal
and that early mobility is anticipated promotes ac-ceptance of the device.
After the external
fixator is applied, the extremity is elevated to reduce swelling. If there are
sharp points on the fixator or pins, they are covered to prevent device-induced
injuries. The nurse monitors the neurovascular status of the extremity every 2
to 4 hours and assesses each pin site for redness, drainage, tenderness, pain,
and loosening of the pin. Some serous drainage from the pin sites is to be
expected. The nurse must be alert for potential problems caused by pressure
from the device on the skin, nerves, or blood vessels and for the development
of compartment syn-drome. The nurse carries out pin care as prescribed to
prevent pin tract infection. This typically includes cleaning each pin site
separately three times a day with cotton-tipped ap-plicators soaked in sterile
saline solution. Crusts should not form at the pin site. If signs of infection
are present or if the pins or clamps seem loose, the nurse notifies the
physician.
The nurse encourages isometric and active exercises
within the limits of tissue damage. When the swelling subsides, the nurse helps
the patient to become mobile within the prescribed weight-bearing limits
(non–weight bearing to full weight bearing). Adherence to weight-bearing
instructions minimizes the chance of loosening of the pins when stress is
applied to the bone–pin in-terface. The fixator is removed after the soft tissue
heals. The frac-ture may require additional stabilization by a cast or molded
orthosis while healing.
The Ilizarov external
fixator is a special device used to correct angulation and rotational defects,
to treat nonunion (failure of bone fragments to heal), and to lengthen limbs.
Tension wires are attached to fixator rings, which are joined by telescoping
rods. Bone formation is stimulated by prescribed daily adjustment of the
telescoping rods. It is important to teach the patient how to adjust the telescoping
rods and how to perform skin care. Gen-erally, the nurse can encourage weight
bearing. After the desired correction has been achieved, no additional
adjustments are made, and the fixator is left in place until the bone heals.
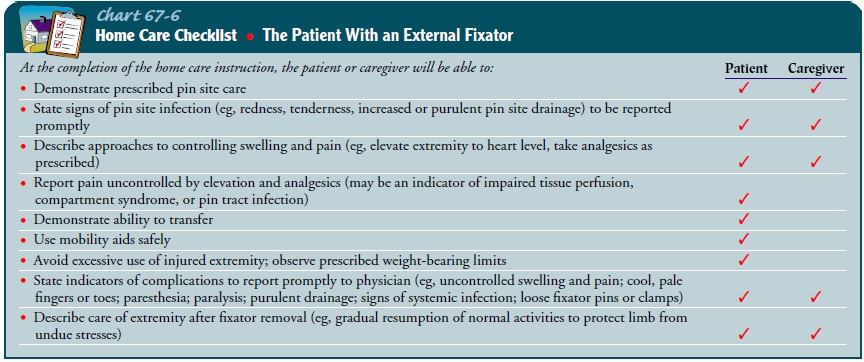
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching the Patient Self-Care.
The nurse teaches
the patient toperform pin site care according to the prescribed protocol (clean
technique can be used at home [McKenzie, 1999]) and to report promptly any
signs of pin site infection: redness, tenderness, in-creased or purulent pin
site drainage, or fever. The nurse also in-structs the patient and family to
monitor neurovascular status and report any changes promptly. The nurse teaches
the patient or family member to check the integrity of the fixator frame daily
and to report loose pins or clamps. A physical therapy referral is help-ful in
teaching the patient how to transfer, use ambulatory aids safely, and adjust to
weight-bearing limits and altered gait pat-terns (Chart 67-6).
Related Topics