Chapter: Medical Surgical Nursing: Musculoskeletal Care Modalities
Total Hip Replacement - Managing the Patient Undergoing Orthopedic Surgery
TOTAL HIP REPLACEMENT
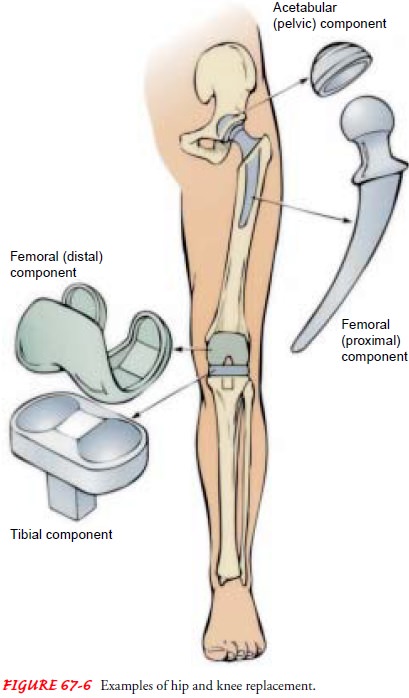
Total hip replacement is
the replacement of a severely damaged hip with an artificial joint. Indications
for this surgery include arthritis (degenerative joint disease, rheumatoid
arthritis), femoral neck fractures, failure of previous reconstructive
surgeries (failed pros-thesis, osteotomy),
and problems resulting from congenital hip disease. A variety of total hip
prostheses are available. Most consist of a metal femoral component topped by a
spherical ball fitted into a plastic acetabular socket (see Fig. 67-6). The
surgeon selects the prosthesis that is most suited to the individual patient,
considering various factors, including skeletal structure and activity level.
The patient is usually 60 years of age or older and has
un-remitting pain or irreversibly damaged hip joints. With the ad-vent of
improved prosthetic materials and operative techniques, the life of the
prosthesis has been extended, and today younger patients with severely damaged
and painful hip joints are under-going total hip replacement.
Nursing Interventions
The nurse must be aware of and monitor for specific
potential complications associated with total hip replacement. Complica-tions
that may occur include dislocation of the hip prosthesis, excessive wound
drainage, thromboembolism, infection, and heel pressure ulcer. Other
complications for which the nurse must monitor include those associated with
immobility, heterotophicossification (formation
of bone in the periprosthetic space), avas-cular necrosis (bone death caused by
loss of blood supply), and loosening of the prosthesis.
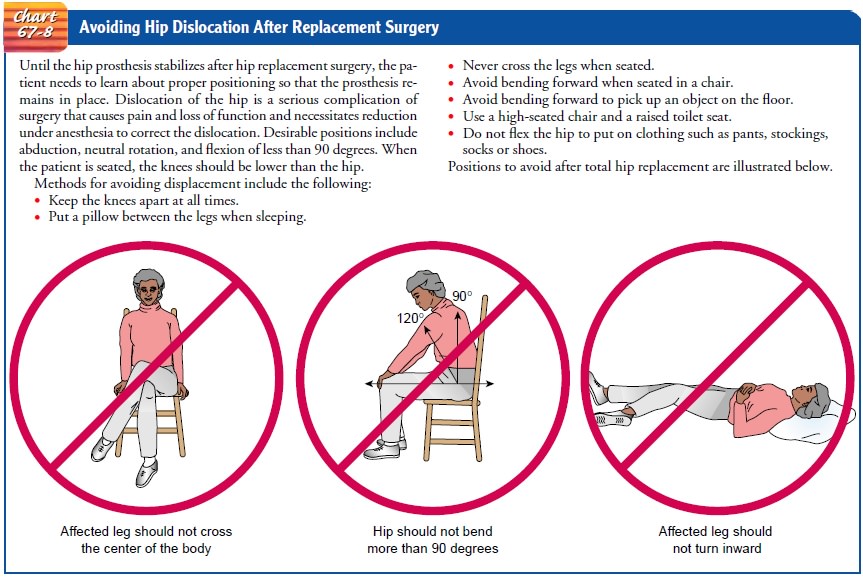
PREVENTING DISLOCATION OF THE HIP PROSTHESIS
Maintenance of the
femoral head component in the acetabular cup is essential. The nurse teaches
the patient about positioning the leg in abduction,
which helps to prevent dislocation of the prosthesis. The use of an abduction
splint, a wedge pillow (Fig. 67-7), or two or three pillows between the legs
keeps the hip in ab-duction. When the nurse turns the patient in bed, it is
important to keep the operative hip in abduction. Depending on the sur-geon’s
preference, some patients are not permitted to be turned onto the affected
side, whereas others may be turned to either side.

The patient’s hip is never flexed more than 90 degrees.
To pre-vent hip flexion, the nurse does not elevate the head of the bed more
than 60 degrees. For use of the fracture bedpan, the nurse instructs the
patient to flex the unaffected hip and to use the trapeze to lift the pelvis
onto the pan. The patient is also re-minded not to flex the affected hip.
Limited flexion is maintained during transfers and when sit-ting. When the patient is initially assisted out of bed, an abduc-tion splint or pillows are kept between the legs.
The nurse encourages the patient
to keep the affected hip in extension, in-structing the patient to pivot on the
unaffected leg with assistance by the nurse, who protects the affected hip from
adduction, flex-ion, internal or
external rotation, and excessive weight bearing.
High-seat (orthopedic) chairs, semireclining wheelchairs,
and raised toilet seats may be used to minimize hip joint flexion. When
sitting, the patient’s hips should be higher than the knees. The patient’s
affected leg should not be elevated when sitting. The patient may flex the
knee.
The nurse teaches the
patient protective positioning, which in-cludes maintaining abduction and
avoiding internal and external rotation, hyperextension, and acute flexion. A
cradle boot may be used to prevent leg rotation and to support the heel off the
bed, preventing development of a pressure ulcer. The patient should use pillows
between the legs when in a supine or side-lying posi-tion and when turning.
Generally, the nurse instructs the patient not to sleep on the side on which
the surgery was performed with-out consulting the surgeon. At no time should
the patient cross his or her legs. The patient must avoid acute flexion of the
hip. The patient should not bend at the waist to put on shoes and socks. Occupational
therapists can provide the patient with devices to as-sist with dressing below
the waist. Hip precautions are needed for about 4 months after surgery (Chart
67-8).
Dislocation may occur with positioning that exceeds the
lim-its of the prosthesis. The nurse must recognize dislocation of the
prosthesis. Indicators are as follows:
·
Increased pain at the surgical
site, swelling, and immobi-lization
·
Acute groin pain in affected
hip or increased discomfort
·
Shortening of the leg
·
Abnormal external or internal
rotation
·
Restricted ability or
inability to move leg
·
Reported “popping” sensation
in hip
If a prosthesis becomes dislocated, the nurse (or the
patient, if at home) immediately notifies the surgeon, because the hip must be
reduced and stabilized promptly so that the leg does not sus-tain circulatory
and nerve damage. After closed reduction, the hip may be stabilized with Buck’s
traction or a brace to prevent re-current dislocation. As the muscles and joint
capsule heal, the chance of dislocation diminishes. Stresses to the new hip
joint should be avoided for the first 3 to 6 months.
MONITORING WOUND DRAINAGE
Fluid and blood accumulating at the surgical site are usually drained with a portable suction device. This prevents accumulation of fluid, which could contribute to discomfort and
provide a site for infection. Drainage of 200 to 500 mL in the first 24 hours
is expected; by 48 hours postoperatively, the total drainage in 8 hours usually
decreases to 30 mL or less, and the suction device is then removed. The nurse
promptly notifies the physician of any drainage volumes greater than
anticipated.
If extensive blood loss is anticipated after total joint
replace-ment surgery, an autotransfusion drainage system (in which the drained blood
is filtered and reinfused into the patient during the immediate postoperative
period) may be used to decrease the need for homologous blood transfusions.
PREVENTING DEEP VEIN THROMBOSIS
The risk for
thromboembolism is particularly great after recon-structive hip surgery. The
incidence of DVT is 45% to 70%. The peak occurrence is 5 to 7 days after
surgery. About 20% of pa-tients with DVT develop pulmonary emboli, of which
about 1% to 3% of cases are fatal. Therefore, the nurse must institute pre-ventive
measures and monitor the patient closely for the devel-opment of DVT and
pulmonary emboli. Signs of DVT include calf pain, swelling, and tenderness.
Measures to promote circula-tion and decrease venous stasis are priorities for
the patient un-dergoing hip reconstruction. The nurse encourages the patient to
consume adequate amount of fluids, to perform ankle and foot exercises hourly
while awake, to use elastic stockings and sequential compression devices as
prescribed, and to transfer out of bed and ambulate with assistance beginning
on the first postoperative day. Low-dose heparin or enoxaparin (Lovenox) is
frequently prescribed as prophylaxis for DVT after hip replacement surgery.
PREVENTING INFECTION
Infection, a serious
complication of total hip replacement, may ne-cessitate removal of the implant.
Patients who are elderly, obese, or poorly nourished and patients who have
diabetes, rheumatoid arthritis, concurrent infections (eg, urinary tract
infection, dental abscess), or large hematomas are at high risk for infection.
Because total joint infections are so disastrous, all
efforts are undertaken to minimize their occurrence. Potential sources of
infection are avoided. Prophylactic antibiotics are prescribed. If indwelling
urinary catheters or portable wound suction devices are used, they are removed
as soon as possible to avoid infection. Prophylactic antibiotics are prescribed
if the patient needs any fu-ture surgical instrumentation, such as tooth
extraction or cysto-scopic examination.
Acute infections may occur within 3 months after surgery and are associated with progressive superficial infections or hematomas. Delayed surgical infections may appear 4 to 24 months after surgery and may cause return of discomfort in the hip. Infections occurring more than 2 years after surgery are attributed to the spread of in-fection through the bloodstream from another site in the body. If an infection occurs, antibiotics are prescribed. Severe infections may require surgical débridement or removal of the prosthesis (Nursing Research Profile 67-1).
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching the Patient Self-Care.
Before
the patient prepares toleave the acute care setting, the nurse provides a
thorough teaching program to promote continuity of the therapeutic regimen and
ac-tive participation in the rehabilitation process (Chart 67-9). The nurse
advises the patient of the importance of the daily exercise program in
maintaining the functional motion of the hip joint and strengthening the
abductor muscles of the hip, and reminds the pa-tient that it will take time to
strengthen and retrain the muscles.
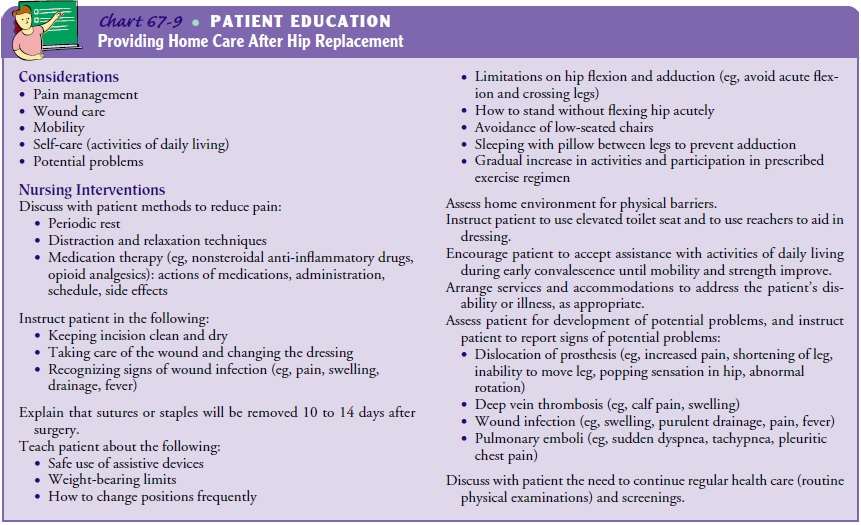
Assistive devices
(crutches, walker, or cane) are used for a time. After sufficient muscle tone
has developed to permit a normal gait without discomfort, these devices are not
necessary. In general, by 3 months, the patient can resume routine ADLs. Stair
climbing is permitted as prescribed and is kept to a minimum for 3 to 6 months.
Frequent walks, swimming, and use of a high rocking chair are ex-cellent for
hip exercises. Sexual activities should be carried out with the patient in the
dependent position (flat on the back) for 3 to 6 months to avoid excessive
adduction and flexion of the new hip.
At no time during the
first 4 months should the patient cross the legs or flex the hip more than 90
degrees. Assistance in putting on shoes and socks may be needed. The patient
should avoid low chairs and sitting for longer than 45 minutes at a time. These
pre-cautions minimize hip flexion and the risks for prosthetic dislo-cation,
hip stiffness, and flexion contracture. Traveling long distances should be
avoided unless frequent position changes are possible. Other activities to
avoid include tub baths, overexertion, jogging, lifting heavy loads, and
excessive bending and twisting (eg, lifting, shoveling snow, forceful turning).
Continuing Care in the Home and Community.
The
nurse maymake a home visit to assess for potential problems and to monitor
wound healing (see Chart 67-9). The nurse, physical therapist, or occupational
therapist assesses the home environment for physical barriers that may impede
the patient’s rehabilitation. In addition, the nurse or therapist may need to
assist the patient in acquiring de-vices, such as reachers to help with
dressing or toilet seat extenders.
After successful surgery and rehabilitation, the patient
can ex-pect a hip joint that is free or almost free of pain, has good mo-tion,
is stable, and permits normal or near-normal ambulation (see Plan of Nursing
Care).
Related Topics