Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Disorders
Acute Low Back Pain
Common
Musculoskeletal Problems
ACUTE LOW BACK PAIN
The number of medical visits resulting from low back pain
is sec-ond only to the number of visits for upper respiratory illnesses. Most
low back pain is caused by one of many musculoskeletal problems, including
acute lumbosacral strain, unstable lum-bosacral ligaments and weak muscles,
osteoarthritis of the spine, spinal stenosis, intervertebral disk problems, and
unequal leg length.
Older patients may experience back pain associated with
os-teoporotic vertebral fractures or bone metastasis. Other causes in-clude
kidney disorders, pelvic problems, retroperitoneal tumors, abdominal aneurysms,
and psychosomatic problems.
In addition, obesity, stress, and occasionally depression
may contribute to low back pain. Back pain due to musculoskeletal disorders
usually is aggravated by activity, whereas pain due to other conditions is not.
Patients with chronic low back pain may develop a dependence on alcohol or
analgesics in an attempt to cope with and self-treat the pain.
Pathophysiology
The spinal column can be considered as an elastic rod
constructed of rigid units (vertebrae) and flexible units (intervertebral
disks) held together by complex facet joints, multiple ligaments, and
paravertebral muscles. Its unique construction allows for flexibil-ity while
providing maximum protection for the spinal cord. The spinal curves absorb
vertical shocks from running and jumping. The trunk muscles help to stabilize
the spine. The abdominal and thoracic muscles are important in lifting
activities. Disuse weakens these supporting structures. Obesity, postural
problems, struc-tural problems, and overstretching of the spinal supports may
re-sult in back pain.
The intervertebral disks
change in character as a person ages. A young person’s disks are mainly
fibrocartilage with a gelatinous matrix. As a person ages, the disks become
dense, irregular fibro-cartilage. Disk degeneration is a common cause of back
pain. The lower lumbar disks, L4–L5 and L5–S1, are subject to the great-est
mechanical stress and the greatest degenerative changes. Disk protrusion
(herniated nucleus pulposus) or facet joint changes can cause pressure on nerve
roots as they leave the spinal canal, which results in pain that radiates along
the nerve.
Clinical Manifestations
The patient complains of
either acute back pain or chronic back pain (lasting more than 3 months without
improvement) and fa-tigue. The patient may report pain radiating down the leg,
which is known as radiculopathy or sciatica and which suggests nerve root
involvement. The patient’s gait, spinal mobility, reflexes, leg length, leg
motor strength, and sensory perception may be altered. Physical examination may
disclose paravertebral muscle spasm (greatly increased muscle tone of the back
postural muscles) with a loss of the normal lumbar curve and possible spinal
deformity.
Assessment and Diagnostic Findings
The Agency for Heath Care Policy and Research developed
guide-lines for assessment and management of acute low back pain (Bigos et al.,
1994). These safe, conservative, and cost-effective guidelines have reduced the
use of noneffective therapeutic inter-ventions, including prolonged bed rest.
The initial evaluation
of acute low back pain includes a focused history and physical examination,
including general observation of the patient, back examination, and neurologic
testing (reflexes, sen-sory impairment, straight-leg raising, muscle strength,
and muscle atrophy). The findings suggest either nonspecific back symptoms or
potentially serious problems, such as sciatica, spine fracture, can-cer,
infection, or rapidly progressing neurologic deficit. If the ini-tial
examination does not suggest a serious condition, no additional testing is
performed during the first 4 weeks of symptoms.
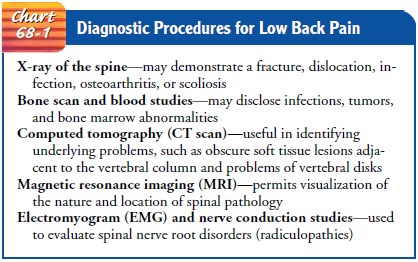
The diagnostic procedures described in Chart 68-1 may be
in-dicated for the patient with potentially serious or prolonged low back pain.
The nurse prepares the patient for these studies, pro-vides the necessary
support during the testing period, and moni-tors the patient for any adverse
responses to the procedures.
Medical Management
Most back pain is self-limited and resolves within 4
weeks with analgesics, rest, stress reduction, and relaxation. Based on initial
assessment findings, the patient is reassured that the assessment indicates
that the back pain is not due to a serious condition. Management focuses on
relief of pain and discomfort, activity modification, and patient education.
Nonprescription analgesics (acetaminophen, ibuprofen) are
usually effective in achieving pain relief. At times, a patient may require the
addition of muscle relaxants or opioids. Heat or cold therapy frequently
provides temporary relief of symptoms. In the absence of symptoms of disease
(radiculopathy of the roots of spinal nerves), manipulation may be helpful.
Other physical modalities have no proven efficacy in treating acute low back pain. They include traction, massage, diathermy, ultrasound, cutaneous laser treatment, biofeedback, and tran-scutaneous electrical nerve stimulation. Likewise, acupuncture and injection procedures have no proven efficacy (Bigos et al., 1994).
Most patients need to alter their activity patterns to
avoid ag-gravating the pain. Twisting, bending, lifting, and reaching, all of
which stress the back, are avoided. The patient is taught to change position
frequently. Sitting should be limited to 20 to 50 minutes based on level of
comfort. Bed rest is recommended for 1 to 2 days, with a maximum of 4 days only
if pain is severe. A grad-ual return to activities and low-stress aerobic
exercise is recom-mended. Conditioning exercises for the trunk muscles are
begun after about 2 weeks.
If there is no improvement within 1 month, additional
assess-ments for physiologic abnormalities are performed. Management is based
on findings.
Related Topics