Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Disorders
Nursing Process: The Patient With Acute Low Back Pain
NURSING PROCESS: THE PATIENT WITH
ACUTE LOW BACK PAIN
Assessment
The nurse encourages the
patient with low back pain to describe the discomfort (eg, location, severity,
duration, characteristics, radiation, associated weakness in the legs).
Descriptions of how the pain occurred—with a specific action (eg, opening a
garage door) or with an activity in which weak muscles were overused (eg,
weekend gardening)—and how the patient has dealt with the pain often suggest
areas for intervention and patient teaching.
If back pain is a recurrent problem, information about
previ-ous successful pain control methods helps in planning current management.
The nurse also asks how the back pain affects the patient’s lifestyle.
Information about work and recreational ac-tivities helps to identify areas for
back health education. Because stress and anxiety can evoke muscle spasms and
pain, the nurse needs insight into environmental variables, work situations,
and family relationships. In addition, the nurse assesses the effect of chronic
pain on the emotional well-being of the patient. Referral to a psychiatric
nurse clinician for assessment and management of stressors contributing to the
low back pain and related depres-sion may be appropriate.
During the interview, the nurse observes the patient’s
posture, position changes, and gait. Often, the patient’s movements are
guarded, with the back kept as still as possible. The patient often selects a
chair of standard seat height with arms for support. The patient may sit and
stand in an unusual position, leaning away from the most painful side, and may
ask for assistance when un-dressing for the physical examination.
On physical examination,
the nurse assesses the spinal curve, any leg length discrepancy, and pelvic
crest and shoulder symmetry. The nurse palpates the paraspinal muscles and
notes spasm and tenderness. When the patient is in a prone position, the
paraspinal muscles relax, and any deformity caused by spasm sub-sides. The
nurse asks the patient to bend forward and then later-ally and notes any
discomfort or limitations in movement. It is important to determine the effect
of these limitations in move-ment on activities of daily living (ADLs). The
nurse evaluates nerve involvement by assessing deep tendon reflexes, sensations
(eg, paresthesia), and muscle strength. Back and leg pain on straight-leg
raising (with the patient supine, the patient’s leg is lifted upward with the
knee extended) suggests nerve root in-volvement. Obesity can contribute to low
back pain. If the patient is obese, the nurse completes a nutritional
assessment.
Nursing Diagnoses
Based on the assessment data, the patient’s major nursing
diag-noses may include the following:
·
Acute pain related to
musculoskeletal problems
·
Impaired physical mobility
related to pain, muscle spasms, and decreased flexibility
·
Deficient knowledge related to
back-conserving techniques of body mechanics
·
Risk for situational low
self-esteem related to impaired mo-bility, chronic pain, and altered role
performance
·
Imbalanced nutrition: more
than body requirements related to obesity
Planning and Goals
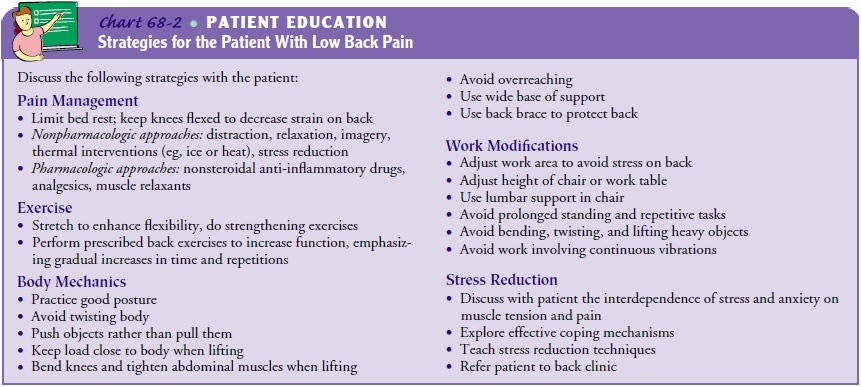
The major goals for the patient may include relief of
pain, im-proved physical mobility, use of back-conserving techniques of body
mechanics, improved self-esteem, and weight reduction (Chart 68-2).
Nursing Interventions
RELIEVING PAIN
To relieve pain, the
nurse encourages the patient to reduce stress on the back muscles and to change
position frequently. Patients are taught to control and modify the perceived
pain through be-havioral therapies that reduce muscular and psychological
ten-sion. Diaphragmatic breathing and relaxation help reduce muscle tension
contributing to low back pain. Diverting the patient’s at-tention from the pain
to another activity (eg, reading, conversa-tion, watching television) may be
helpful in some instances. Guided imagery, in which the relaxed patient learns
to focus on a pleasant event, may be used along with other pain-relief
strate-gies (see Chart 68-2).
If medication is prescribed, the nurse assesses the
patient’s re-sponse to each medication. As the acute pain subsides,
medica-tions are reduced as prescribed. Self-applied intermittent heat or cold
may reduce the pain. The nurse evaluates and notes the pa-tient’s response to
various pain management modalities.
IMPROVING PHYSICAL MOBILITY
Physical mobility is monitored through continuing assessments. The nurse assesses how the patient moves and stands. As the back pain subsides, self-care activities are resumed with minimal strain on the injured structures. Position changes should be made slowly and carried out with assistance as required. Twisting and jarring motions are avoided.
The nurse encourages the patient to alternate lying, sitting, and walking activities frequently
and advises the patient to avoid sitting, standing, or walking for long
periods. The patient may find that sitting in a chair with arm rests to
sup-port some of the body weight and a soft support at the small of the back
provides comfort.
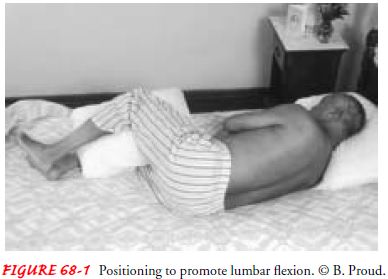
With severe pain, the patient limits activity for 1 to 2
days. Extended periods of inactivity are not effective and result in
de-conditioning. The patient rests in bed on a firm, nonsagging mattress (a bed
board may be used). Lumbar flexion is increased by elevating the head and
thorax 30 degrees using pillows or a foam wedge and slightly flexing the knees
supported on a pillow. Alternatively, the patient assumes a lateral position
with knees and hips flexed (curled position) with a pillow between the knees
and legs and a pillow supporting the head (Fig. 68-1). A prone position is
avoided because it accentuates lordosis. The nurse in-structs the patient to
get out of bed by rolling to one side and placing the legs down while pushing
the torso up, keeping the back straight.
As the patient achieves comfort, activities are gradually re-sumed, and an exercise program is initiated. Initially, low-stress aerobic exercises, such as short walks or swimming, are suggested. After 2 weeks, conditioning exercises for the abdominal and trunk muscles are started.
The physical therapist designs an
exercise program for the individual patient to reduce lordosis, increase
flexibility, and reduce strain on the back. It may include hyper-extension
exercises to strengthen the paravertebral muscles, flexion exercises to
increase back movement and strength, and isometric flexion exercises to
strengthen trunk muscles. Each ex-ercise period begins with relaxation.
Exercise begins gradually and increases as the patient recovers.
The nurse encourages the
patient to adhere to the prescribed exercise program. Erratic exercising is
ineffective. For most exer-cise programs, it is suggested that the person
exercise twice a day, increasing the number of exercises gradually. Some
patients may find it difficult to adhere to a program of prescribed exercises
for a long period. These patients are encouraged to improve their posture, use
good body mechanics on a regular basis, and engage in regular exercise
activities (eg, walking, swimming) to maintain a healthy back. Activities
should not cause excessive lumbar strain, twisting, or discomfort; for example,
activities such as horseback riding and weight-lifting are avoided.
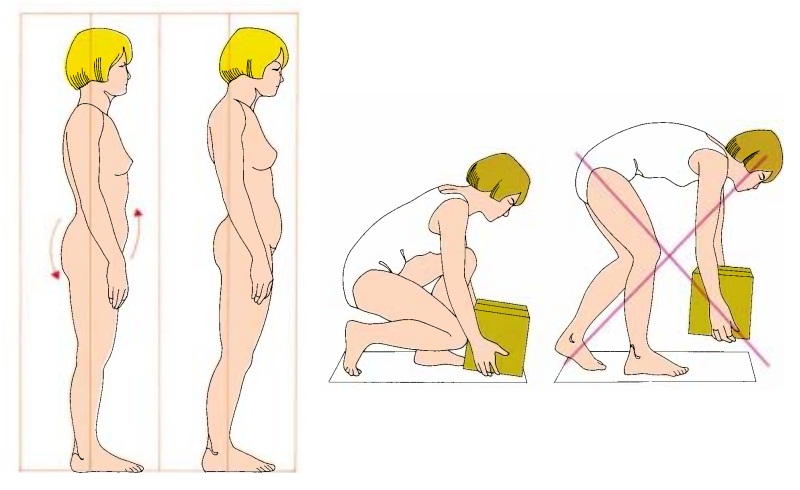
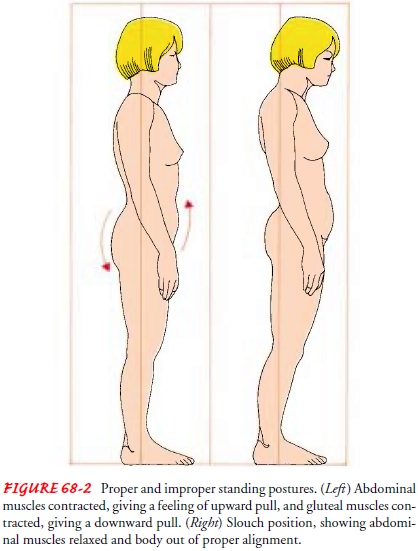
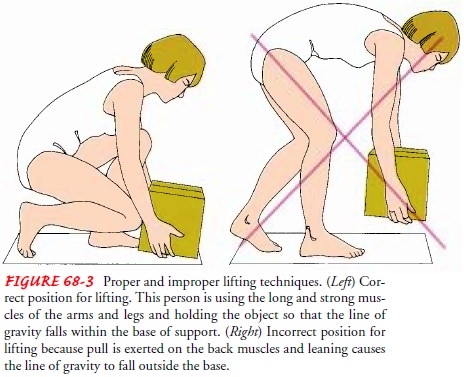
USING PROPER BODY MECHANICS
Good body mechanics and
posture are essential to avoid recur-rence of back pain. The patient must be
taught how to stand, sit, lie, and lift properly (Figs. 68-2 and 68-3).
Providing the patient with a list of suggestions helps in making these
long-term changes (Chart 68-3). The patient who wears high heels is en-couraged
to change to low heels. The patient who is required to stand for long periods
should shift weight frequently and should rest one foot on a low stool, which
decreases lumbar lordosis. The proper posture can be verified by looking in a
mirror to see whether the chest is up and the abdomen is tucked in. Locking the
knees when standing is avoided, as is bending forward for long periods.
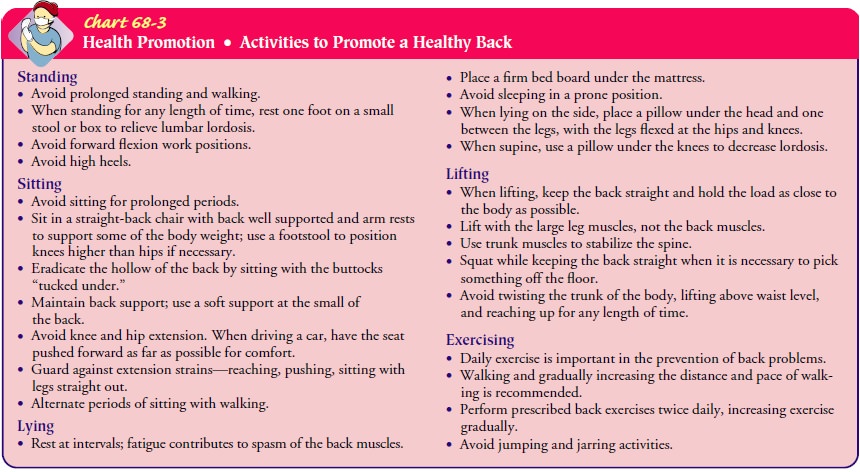
When the patient is sitting, the knees and hips should be flexed, and the knees should be level with the hips or higher to minimize lordosis. The feet should be flat on the floor. The back needs to be supported. The patient should sleep on the side with knees and hips flexed, or supine with knees supported in a flexed position. Sleeping prone should be avoided.
The nurse instructs the patient in the safe and correct
way to lift objects—using the strong quadriceps muscles of the thighs, with
minimal use of weak back muscles. With feet placed to pro-vide a wide base of
support, the patient should bend the knees, tighten the abdominal muscles, and
lift the object close to the body with a smooth motion, avoiding twisting and
jerking. To prevent recurrence of acute low back pain, the nurse may instruct
the patient to wear a back support when repeated lifting is re-quired and to
avoid lifting more than one third of his or her weight without help.
It takes about 6 months for a person to readjust postural
habits. Practicing these protective and defensive postures, positions, and body
mechanics results in natural strengthening of the back and diminishes the
chance that back pain will recur.
IMPROVING SELF-ESTEEM
Because of the
immobility associated with low back pain, the pa-tient may depend on others to
do various tasks. Dependency may continue beyond physiologic needs and become a
way to fulfill psychosocial needs. Assisting both the patient and support
peo-ple to recognize continued dependency helps the patient identify and cope
with the underlying reason for the dependency.
Role-related responsibilities may have been modified with
the onset of low back pain. As recovery from acute low back pain and immobility
progresses, the patient may resume former role-related responsibilities.
If these activities contributed to the development of low back pain, however, it may be difficult to resume them without chronic low back pain syndrome, with associated disability and depres-sion resulting.
If the patient experiences secondary gains associated with low back disability (eg, worker’s compensation,
easier lifestyle or workload, increased emotional support), a “low back
neurosis” may develop. The patient may need help in coping with specific
stressors and in learning how to control stressful situa-tions. When people
successfully deal with stress, they develop confidence in their abilities to
manage other stressful situations. Psychotherapy or counseling may be needed to
assist the person in resuming a full, productive life. Back clinics use
multidiscipli-nary approaches to help the patient with pain and with
resump-tion of role-related responsibilities.
MODIFYING NUTRITION FOR WEIGHT REDUCTION
Obesity contributes to back strain by stressing the relatively weak back muscles. Exercises are less effective and more difficult to per-form when the patient is overweight. Weight reduction through diet modification may prevent recurrence of back pain. Weight reduction is based on a sound nutritional plan that includes a change in eating habits to maintain desirable weight. Monitoring weight reduction, noting achievement, and providing encour-agement and positive reinforcement facilitate adherence. Fre-quently, back problems resolve as normal weight is achieved.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include the following:
1) Experiences
pain relief
a) Rests
comfortably
b) Changes
positions comfortably
c) Obtains
relief through use of physical modalities, psycho-logical techniques, and
medications
d) Avoids
drug dependency
2) Demonstrates
resumption of physical mobility
a) Resumes
activities gradually
b) Avoids
positions that cause discomfort and muscle spasm
c) Plans
recumbent rest periods throughout the day
3) Demonstrates
back-conserving body mechanics
a) Improves
posture
b) Positions
self to minimize stress on the back
c) Demonstrates
use of good body mechanics
d) Participates
in exercise program
4) Resumes
role-related responsibilities
a) Uses
coping techniques to deal with stressful situations
b) Demonstrates
decreased dependence on others for self-care
c) Resumes
role responsibilities as low back pain resolves
d) Resumes
full, productive lifestyle
5) Achieves
desired weight
a) Identifies
need to lose weight if appropriate
b) Sets
realistic goals
c) Participates
in development of weight-reduction plan
d) Complies
with weight-reduction regimen
Related Topics