Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Disorders
Osteoporosis - Metabolic Bone Disorders
Metabolic
Bone Disorders
OSTEOPOROSIS
Osteoporosis is a
disease that threatens more than 28 million Americans (National Osteoporosis
Foundation, 2000). Charac-teristics of osteoporosis include a reduction of bone
density and a change in bone structure, both of which increase susceptibility
to fracture. The normal homeostatic bone turnover is altered: the rate of bone
resorption is greater than the rate of bone formation, resulting in a reduced
total bone mass. Suboptimal bone mass de-velopment in children and teens
contributes to the development of osteoporosis. With osteoporosis, the bones
become progres-sively porous, brittle, and fragile; they fracture easily under
stresses that would not break normal bone. Osteoporosis frequently re-sults in
compression fractures (Fig. 68-7) of the thoracic and lum-bar spine, fractures
of the neck and intertrochanteric region of the femur, and Colles’ fractures of
the wrist. The probability that a 50-year-old Caucasian woman will experience a
hip fracture dur-ing her lifetime is 14%; for a Caucasian man, it is 5% to 6%.
The risk for African Americans is lower—6% for women and 3% for men (NIH
Consensus Statement, 2000). Multiple compression fractures of the vertebrae
result in skeletal deformity. Osteoporosis is a costly disorder not only in
terms of health care dollars but also in terms of human suffering, pain,
disability, and death.
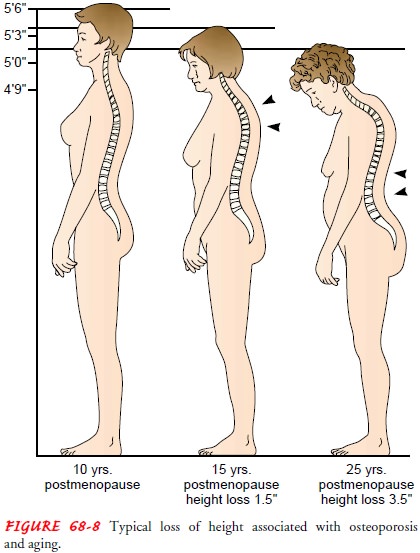
The gradual collapse of a vertebra may be asymptomatic;
it is observed as progressive kyphosis. With the development of kyphosis
(“dowager’s hump”), there is an associated loss of height (Fig. 68-8).
Frequently, postmenopausal women lose height from vertebral collapse. The
postural changes result in relaxation of the abdominal muscles and a protruding
abdomen. The deformity may also produce pulmonary insufficiency. Many patients
com-plain of fatigue.
Prevention
Primary osteoporosis
occurs in women after menopause and later in life in men, but it is not merely
a consequence of aging. Failure to develop optimal peak bone mass during
childhood, adolescence, and young adulthood contributes to the development of
osteo-porosis without resultant bone loss. Early identification of at-risk
teenagers and young adults, increased calcium intake, participation in regular
weight-bearing exercise, and modification of lifestyle (eg, reduced use of
caffeine, cigarettes, and alcohol) are interven-tions that decrease the risk
for development of osteoporosis, frac-tures, and associated disability later in
life. Secondary osteoporosis is the result of medications or other conditions
and diseases that affect bone metabolism. Specific disease states (eg, celiac
disease, hypogonadism) and medications (eg, corticosteroids, antiseizure
medications) that place patients at risk need to be identified and therapies
instituted to reverse the development of osteoporosis.
Gerontologic Considerations
The prevalence of
osteoporosis in women older than 80 years of age is 84% (Genant et al., 1997).
The average 75-year-old woman has lost 25% of her cortical bone and 40% of her
trabecular bone. With the aging of the population, the incidence of fractures
(more than 1.5 million fractures per year), pain, and disability as-sociated
with osteoporosis is rising. The mortality rate 1 year after hip fracture is
20%. Two-thirds of patients with hip fracture never regain their prefracture
level of functioning (NIH Consensus Statement, 2000).
Elderly people absorb dietary calcium less efficiently and ex-crete it more readily through their kidneys; therefore, post-menopausal women and the elderly actually need to consume liberal amounts of calcium. As much as 1500 mg daily for post-menopausal women may be prescribed. Most residents of long-term care facilities have a low bone mineral density (BMD) and are at risk for fracture. Hip protectors have been found to reduce the incidence of hip fracture in the elderly; however, compliance in wearing these hip protectors is low (Kannus et al., 2000).
Pathophysiology
Normal bone remodeling
in the adult results in gradually in-creased bone mass until the early 30s.
Gender, race, genetics, aging, low body weight and body mass index, nutrition,
lifestyle choices (eg, smoking, caffeine and alcohol consumption), and physical
activity influence peak bone mass and the development of osteoporosis (Fig.
68-9). Although the consequences of osteo-porosis (eg, fractures) occur with
aging, osteoporosis is not a dis-ease of the elderly. Rather, its onset occurs
earlier in life, when bone mass peaks and then begins to decline.
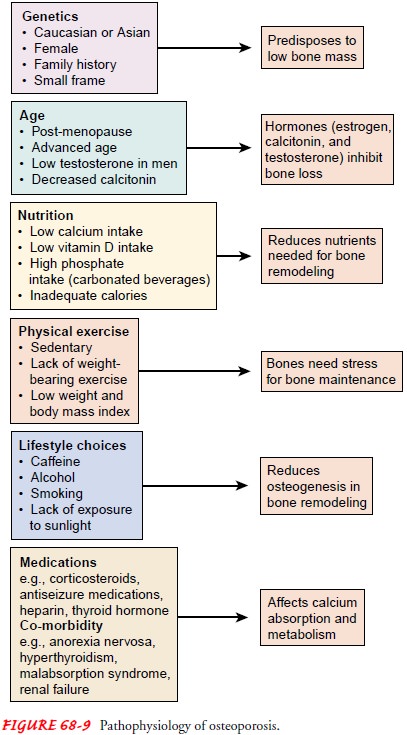
Loss of bone mass is a
universal phenomenon associated with aging. Age-related loss begins soon after
the peak bone mass is achieved (ie, in the fourth decade). Calcitonin, which
inhibits bone resorption and promotes bone formation, is decreased. Es-trogen,
which inhibits bone breakdown, decreases with aging. On the other hand,
parathyroid hormone (PTH) increases with aging, increasing bone turnover and
resorption. The consequence of these changes is net loss of bone mass over
time.
The withdrawal of estrogens at menopause or with oophorec-tomy causes an accelerated bone resorption that continues dur-ing the postmenopausal years. Women develop osteoporosis more frequently and more extensively than men because of lower peak bone mass and the effect of estrogen loss during menopause. More than half of all women older than 45 years of age show ev-idence of osteopenia. World Health Organization (WHO) diag-nostic categories for osteoporosis are based on BMD scan findings (Walker-Bone et al., 2001).
Secondary osteoporosis
is associated with many disease states, nutritional deficiencies, and
medications. Coexisting medical conditions (eg, malabsorption syndromes,
lactose intolerance, alcohol abuse, renal failure, liver failure, Cushing’s
syndrome, hyperthyroidism, and hyperparathyroidism) contribute to bone loss and
the development of osteoporosis. Medications (eg, cortico-steroids, antiseizure
medications, heparin, tetracycline, aluminum-containing antacids, and thyroid
supplements) affect the body’s use and metabolism of calcium. The degree of
osteoporosis is re-lated to the duration of medication therapy. When the
therapy is discontinued or the metabolic problem is corrected, the progres-sion
of osteoporosis is halted, but restoration of lost bone mass usually does not
occur.
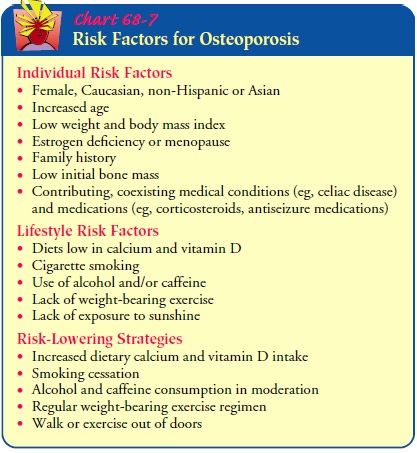
Risk Factors
Small-framed, nonobese
Caucasian women are at greatest risk for osteoporosis. Also, Asian women of
slight build are at risk for low peak BMD. African American women, who have a
greater bone mass than Caucasian women, are less susceptible to osteoporosis.
Men have a greater peak bone mass and do not experience sudden estrogen reduction.
As a result, osteoporosis occurs in men at a lower rate and at an older age
(about one decade later). How-ever, it has been determined that testosterone
and estrogen are important in achieving and maintaining bone mass in men.
Nutritional factors contribute to the development of
osteo-porosis. A balanced diet—including adequate calories and nutri-ents
needed to maintain bone, calcium, and vitamin D—must be consumed. Vitamin D is
necessary for calcium absorption and for normal bone mineralization. Dietary
calcium and vitamin D must be adequate to maintain bone remodeling and body
func-tions. The best source of calcium and vitamin D is fortified milk. A cup
of milk or calcium-fortified orange juice contains about 300 mg of calcium.
The recommended adequate
intake (AI) level of calcium for the age range of puberty through young
adulthood (9 to 19 years of age) is 1300 mg per day. The goal of this daily
level of calcium is to maximize peak bone mass. The AI level for adults 19 to
50 years of age is 1000 mg per day, and the AI level for adults 51 years and
older is 1200 mg per day. The actual estimated aver-age daily intake is 300 to
500 mg. The recommended adult vita-min D intake is 400 to 600 IU per day.
Inadequate intake of calcium or vitamin D over a period of years results in
decreased bone mass and the development of osteoporosis.
Bone formation is
enhanced by the stress of weight and mus-cle activity. Resistance and impact
exercises are most beneficial in developing and maintaining bone mass. Immobility
contributes to the development of osteoporosis. When immobilized by casts,
general inactivity, paralysis or other disability, the bone is re-sorbed faster
than it is formed, and osteoporosis results. Risk fac-tors for osteoporosis are
summarized in Chart 68-7.
Assessment and Diagnostic Findings
Osteoporosis may be identified on routine x-rays when there has been 25% to 40% demineralization. There is radiolucency to the bones. When the vertebrae collapse, the thoracic vertebrae become wedge-shaped and the lumbar vertebrae become biconcave.
Osteoporosis is diagnosed by dual-energy
x-ray absorptiometry (DEXA), which provides information about BMD at the spine
and hip. The DEXA scan data are analyzed and reported as T-scores (the number
of standard deviations [SD] above or below the average BMD value for a young,
healthy Caucasian woman). A normal BMD is less than 1 SD below the young adult
mean value. The WHO defines osteoporosis as being present when the T-score is
at least 2.5 SD below the young adult mean value. Osteopenia is diagnosed when
the BMD T-score is between 1 and 2.5 SD below the young adult mean value
(Walker-Bone et al., 2001). Fracture risk increases progressively as the SD of
the T-score falls below the mean value.
Quantitative ultrasound studies (QUS) of the heel also
are used to diagnose osteoporosis and to predict the risk of hip and
nonvertebral fracture. When standardization of sites and compa-rability of
findings of BMD and QUS are determined, these mea-surements will become more
clinically useful (NIH Consensus Statement, 2000).
These BMD studies are useful in identifying osteopenic
and osteoporotic bone and in assessing response to therapy. Through early
screening (using both assessment of risk factors and BMD scans), promotion of
adequate dietary intake of calcium and vita-min D, encouragement of lifestyle
changes, and early institution of preventive medications, bone loss and
osteoporosis can be reduced, resulting in a reduced incidence of fracture.
Laboratory studies (eg,
serum calcium, serum phosphate, serum alkaline phosphatase, urine calcium
excretion, urinary hy-droxyproline excretion, hematocrit, erythrocyte
sedimentation rate) and x-ray studies are used to exclude other possible
medical diagnoses (eg, multiple myeloma, osteomalacia, hyperparathy-roidism,
malignancy) that contribute to bone loss.
Medical Management
An adequate, balanced
diet rich in calcium and vitamin D through-out life, with an increased calcium
intake during adolescence, young adulthood, and the middle years, protects
against skeletal demineralization. Such a diet would include three glasses of
skim or whole vitamin D–enriched milk or other foods high in calcium (eg,
cheese and other dairy products, steamed broccoli, canned salmon with bones),
daily. To ensure adequate calcium intake, a calcium supplement (eg, Caltrate,
Citrocal) may be prescribed and taken with meals or with a beverage high in
vitamin C to pro-mote absorption. The recommended daily dose should be split
and not taken as a single dose. Common side effects of calcium supplements are
abdominal distention and constipation.
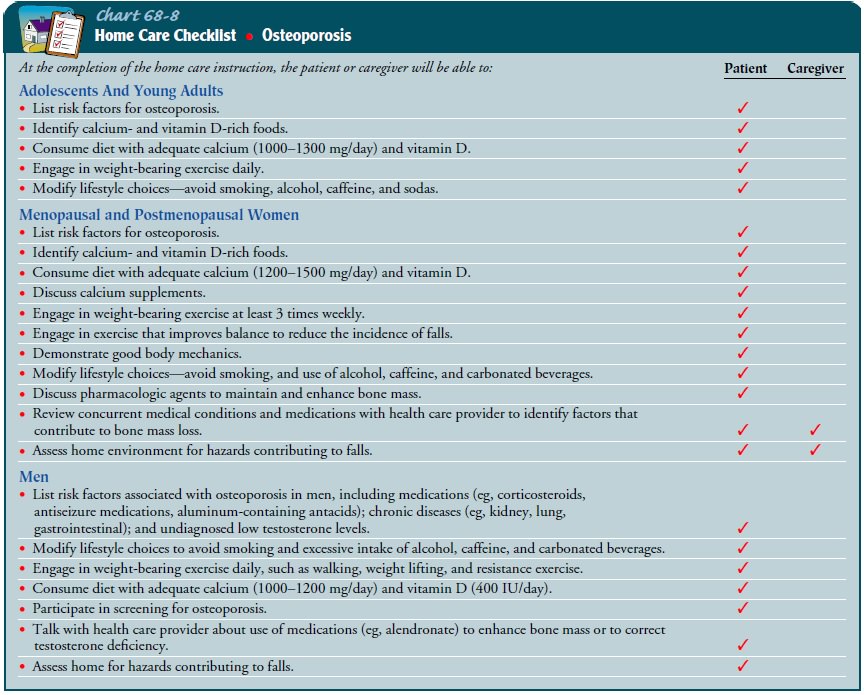
Regular weight-bearing
exercise promotes bone formation. From 20 to 30 minutes of aerobic exercise
(eg, walking), 3 days or more a week, is recommended. Weight training
stimulates an increase in BMD. In addition, exercise improves balance,
reduc-ing the incidence of falls and fractures (Chart 68-8).
PHARMACOLOGIC THERAPY
At natural or surgical
menopause, hormone replacement ther-apy (HRT) with estrogen and progesterone
has been the main-stay of therapy to retard bone loss and prevent occurrence of
fractures. Estrogen replacement decreases bone resorption and increases bone
mass, reducing the incidence of osteoporotic fractures. However, recent studies
have demonstrated greater risks than previously recognized (Chen, Weiss,
Newcomb, Barlow & White, 2002).
Selective estrogen
receptor modulators (SERMs), such as ralox-ifene (Evista), reduce the risk for
osteoporosis by preserving bone mineral density without estrogenic effects on
the uterus. They are indicated for both prevention and treatment of
osteoporosis.
Other medications that
may be prescribed to treat osteoporosis include bisphosphonates (eg,
alendronate [Fosamax]; risedronate [Actonel]) and calcitonin. Alendronate
offers an alternative to HRT and produces increased bone mass (by inhibiting
osteoclast function) and decreased bone loss. Bisphosphonates reduce spine and
hip fractures associated with osteoporosis. A weekly dosage strength of alendronate
is available and has been shown to be as ef-fective as previously used daily
dosing. Adequate calcium and vita-min D intake is needed for maximum effect,
but these supplements should not be taken at the same time of day as
bisphosphonates. Side effects of alendronate include gastrointestinal symptoms
(eg, dyspepsia, nausea, flatulence, diarrhea, constipation). Alen-dronate and
risedronate are approved for the prevention and treat-ment of
glucocorticoid-induced osteoporosis in men and women.
Calcitonin (Miacalcin) primarily suppresses bone loss
through direct action on osteoclasts and reduced bone turnover. It is
ef-fective in increasing BMD. Calcitonin is administered by nasal spray or by
subcutaneous or intramuscular injection. Side effects include nasal irritation,
flushing, gastrointestinal disturbances, and urinary frequency.
Recently, in clinical trials, small daily subcutaneous
injections of PTH or PTH bioactive fragments (1-34; 1-38), or both, have been
found to stimulate bone formation (Neer et al., 2001). U.S. Food and Drug
Administration (FDA) approval of prescription of intermittent PTH is
anticipated as a new anabolic approach to treatment of osteoporosis.
Natural estrogens (plant-derived phytoestrogens) have not
been shown to be effective in reducing osteoporosis-related frac-tures (NIH
Consensus Statement, 2000).
In addition, antilipid medications, such as statins
(HMG-CoA reductase inhibitors), reduce the incidence of fractures in patients
who take these medications to control their hyperlipid-emia. The statins
promote bone growth, thereby preventing the development of osteoporosis.
FRACTURE MANAGEMENT
Fractures of the hip are managed surgically by joint
replacement or by closed or open reduction with internal fixation (eg, hip
pin-ning). Surgery, early ambulation, intensive physical therapy, and adequate
nutrition result in decreased morbidity and improved outcomes. In addition,
patients need to be evaluated for osteo-porosis and treated, if indicated.
Osteoporotic compression fractures of the vertebra are
man-aged conservatively. Additional vertebral fractures and progres-sive
kyphosis are common. Pharmacologic and dietary treatment are aimed at
increasing vertebral bone density. A new procedure, percutaneous
vertebroplasty/kyphoplasty (injection of poly-methylmethacrylate bone cement
into the fractured vertebra), is reported to provide rapid acute pain relief
and improved quality of life. The long-term effect of this procedure is unknown
(NIH Consensus Statement, 2000).
Related Topics