Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Disorders
Nursing Process: The Patient Undergoing Foot Surgery
NURSING PROCESS: THE PATIENT
UNDERGOING FOOT SURGERY
Assessment
Surgery of the foot may
be necessary because of various condi-tions, including neuromas and foot
deformities (bunion, hammer toe, clawfoot). Generally, foot surgery is
performed on an outpa-tient basis. Before surgery, the nurse assesses the patient’s
ambu-latory ability and balance and the neurovascular status of the foot.
Additionally, the nurse considers the availability of assistance at home and
the structural characteristics of the home in planning for care during the
first few days after surgery. The nurse uses these data, in addition to
knowledge of the usual medical management of the condition, to formulate
appropriate nursing diagnoses.
Nursing Diagnoses
Based on the assessment data, the nursing diagnoses for
the pa-tient undergoing foot surgery may include the following:
·
Risk for ineffective
peripheral tissue perfusion: related to swelling
·
Acute pain related to surgery,
inflammation, and swelling
·
Impaired physical mobility
related to the foot-immobilizing device
·
Risk for infection related to
the surgical procedure/surgical incision
Planning and Goals
The goals for the patient may include adequate tissue
perfusion, relief of pain, improved mobility, and absence of infection.
Nursing Interventions
PROMOTING TISSUE PERFUSION
Neurovascular assessment of the exposed toes every 1 to 2
hours for the first 24 hours is essential to monitor the function of the nerves
and the perfusion of the tissues. If the patient is discharged within several
hours after the surgery, the nurse teaches the pa-tient and family how to
assess for swelling and neurovascular status (circulation, motion, sensation).
Compromised neuro-vascular function can increase the patient’s pain.
RELIEVING PAIN
Pain experienced by
patients who undergo foot surgery is related to inflammation and edema.
Formation of a hematoma may con-tribute to the discomfort. To control the
swelling, the foot should be elevated on several pillows when the patient is
sitting or lying. Intermittent ice packs applied to the surgical area during
the first 24 to 48 hours may be prescribed to control swelling and provide some
pain relief. As activity increases, the patient may find that dependent
positioning of the foot is uncomfortable. Simply ele-vating the foot often
relieves the discomfort. Oral analgesics may be used to control the pain. The
nurse instructs the patient and family about appropriate use of these
medications.
IMPROVING MOBILITY
After surgery, the patient will have a bulky dressing on
the foot, protected by a light cast or a special protective boot. Limits for
weight bearing on the foot will be prescribed by the surgeon. Some patients are
allowed to walk on the heel and progress to weight-bearing as tolerated; other
patients are restricted to non– weight-bearing activities. Assistive devices
(eg, crutches, walker) may be needed. The choice of the devices depends on the
pa-tient’s general condition and balance and on the weight-bearing
prescription. Safe use of the assistive devices must be ensured through
adequate patient education and practice before dis-charge. Strategies to move
around the house safely while using assistive devices are discussed with the
patient. As healing pro-gresses, the patient gradually resumes ambulation
within pre-scribed limits. The nurse emphasizes adherence to the therapeutic
regimen.
PREVENTING INFECTION
Any surgery carries a
risk for infection. In addition, percutaneous pins may be used to hold bones in
position, and these pins serve as potential sites for infection. Because the
foot is on or near the floor, care must be taken to protect it from dirt and
moisture. When bathing, the patient can secure a plastic bag over the dress-ing
to prevent it from getting wet. Patient instruction concern-ing aseptic wound
care and pin care may be necessary.
The nurse teaches the patient to monitor for temperature
and infection. Drainage on the dressing, foul odor, or increased pain and
swelling could indicate infection. The nurse instructs the pa-tient to promptly
report any of these findings to the physician. If prophylactic antibiotics are
prescribed, the nurse provides in-struction about their correct use.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
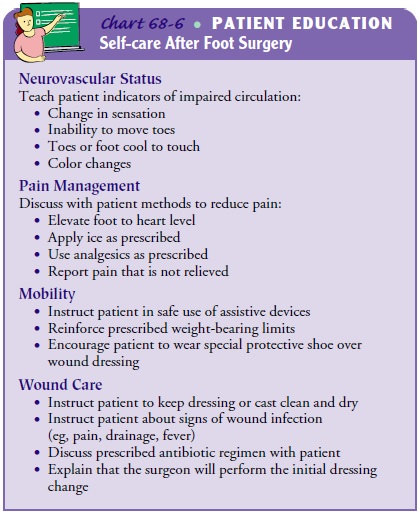
The nurse plans patient teaching for home care, focusing
on neuro-vascular status, pain management, mobility, and wound care (Chart
68-6).
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Maintains
peripheral tissue perfusion
a) Demonstrates
normal skin temperature and capillary refill
b) Exhibits
normal sensations
c) Exhibits
acceptable motor function
2) Obtains
pain relief
a) Elevates
foot to control edema
b) Applies
ice to foot as prescribed
c) Uses
oral analgesics as needed and prescribed
d) Reports
decreased pain and increased comfort
3) Demonstrates
increased mobility
a) Uses
assistive devices safely
b) Resumes
weight-bearing gradually as prescribed
c) Exhibits
diminished disability associated with preoper-ative condition
4) Develops
no infection
a) Reports
temperature and pulse within normal limits
b) Reports
no purulent drainage or signs of wound in-flammation
c) Maintains
clean and dry dressing
d) Takes prophylactic antibiotics as prescribed
Related Topics