Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Disorders
Nursing Process: The Patient With a Bone Tumor
NURSING PROCESS: THE PATIENT WITH A BONE TUMOR
Assessment
The nurse asks the patient about the onset and course of symp-toms. During the interview, the nurse notes the patient’s under-standing of the disease process, how the patient and the family have been coping, and how the patient has managed the pain.
On physical examination, the nurse gently palpates the mass and notes its
size and associated soft tissue swelling, pain, and ten-derness. Assessment of
the neurovascular status and range of motion of the extremity provides baseline
data for future com-parisons. The nurse evaluates the patient’s mobility and
ability to perform ADLs.
Diagnosis
NURSING DIAGNOSES
Based on the nursing
assessment data, the major nursing diagnoses for the patient with a bone tumor
may include the following:
·
Deficient knowledge related to
the disease process and the therapeutic regimen
·
Acute and chronic pain related
to pathologic process and surgery
·
Risk for injury: pathologic
fracture related to tumor and metastasis
·
Ineffective coping related to
fear of the unknown, percep-tion of disease process, and inadequate support
system
·
Risk for situational low
self-esteem related to loss of body part or alteration in role performance
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Potential complications may include the following:
·
Delayed wound healing
·
Nutritional deficiency
·
Infection
·
Hypercalcemia
Planning and Goals
The major goals for the patient include knowledge of the
disease process and treatment regimen, control of pain, absence of patho-logic
fractures, effective patterns of coping, improved self-esteem, and absence of
complications.
Nursing Interventions
The nursing care of a
patient who has undergone excision of a bone tumor is similar in many respects
to that of other patients who have had skeletal surgery. Vital signs are
monitored; blood loss is assessed; and observations are made to assess for the
devel-opment of complications such as deep vein thrombosis, pul-monary emboli,
infection, contracture, and disuse atrophy. The affected part is elevated to
control swelling, and the neurovascu-lar status of the extremity is assessed.
PROMOTING UNDERSTANDING OF THE DISEASE PROCESS AND TREATMENT REGIMEN
Patient and family teaching about the disease process and
diag-nostic and management regimens is essential. Explanation of di-agnostic
tests, treatments (eg, wound care), and expected results (eg, decreased range
of motion, numbness, change of body con-tours) helps the patient deal with the
procedures and changes. Cooperation and adherence to the therapeutic regimen
are en-hanced through understanding. The nurse can most effectively reinforce
and clarify information provided by the physician by being present during these
discussions.
RELIEVING PAIN
Accurate pain assessment
is the foundation for pain management. Pharmacologic and nonpharmacologic pain
management tech-niques are used to relieve pain and increase the patient’s
comfort level. The nurse works with the patient in designing the most
ef-fective pain management regimen, thereby increasing the pa-tient’s control
over the pain. The nurse prepares the patient and gives support during painful
procedures. Prescribed IV or epidural analgesics are used during the early
postoperative period. Later, oral or transdermal opioid or nonopioid analgesics
are usu-ally adequate to relieve pain. In addition, external radiation or
systemic radioisotopes may be used to control pain.
PREVENTING PATHOLOGIC FRACTURE
Bone tumors weaken the bone to a point at which normal
activ-ities or even position changes can result in fracture. During nurs-ing
care, the affected extremities must be supported and handled gently. External
supports (eg, splints) may be used for additional protection. At times, the
patient may elect to have surgery (eg, open reduction with internal fixation,
joint replacement) in an attempt to prevent pathologic fracture. Prescribed
weight-bearing restrictions must be followed. The nurse teaches the patient how
to use assistive devices safely and how to strengthen unaffected extremities.
PROMOTING COPING SKILLS
The nurse encourages the
patient and family to verbalize their fears, concerns, and feelings. They need
to be supported as they deal with the impact of the malignant bone tumor.
Feelings of shock, despair, and grief are expected. Referral to a psychiatric
nurse liaison, psychologist, counselor, or spiritual advisor may be indicated
for specific psychological help and emotional support.
PROMOTING SELF-ESTEEM
Independence versus
dependence is an issue for the patient who has a malignancy. Lifestyle is
dramatically changed, at least tem-porarily. It is important to support the
family in working through the adjustments that must be made. The nurse assists
the patient in dealing with changes in body image due to surgery and possi-ble
amputation. It is helpful to provide realistic reassurance about the future and
resumption of role-related activities and to en-courage self-care and
socialization. The patient participates in planning daily activities. The nurse
encourages the patient to be as independent as possible. Involvement of the
patient and fam-ily throughout treatment encourages confidence, restoration of
self-concept, and a sense of being in control of one’s life.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Delayed Wound Healing
Wound healing may be delayed because of tissue trauma
from surgery, previous radiation therapy, inadequate nutrition, or in-fection.
The nurse minimizes pressure on the wound site to pro-mote circulation to the
tissues. An aseptic, nontraumatic wound dressing promotes healing. Monitoring
and reporting of labora-tory findings facilitate initiation of interventions to
promote homeostasis and wound healing.
Repositioning the patient at frequent intervals reduces
the in-cidence of skin breakdown due to pressure. Special therapeutic beds may
be needed to prevent skin breakdown and to promote wound healing after
extensive surgical reconstruction and skin grafting.
Inadequate Nutrition
Because loss of appetite, nausea, and vomiting are
frequent side effects of chemotherapy and radiation therapy, it is necessary to
provide adequate nutrition for healing and health promotion. Antiemetics and
relaxation techniques reduce the gastrointestinal reaction. Stomatitis is
controlled with anesthetic or antifungal mouthwash. Adequate hydration is
essential. Nu-tritional supplements or total parenteral nutrition may be
pre-scribed to achieve adequate nutrition.
Osteomyelitis and Wound Infections
Prophylactic antibiotics and strict aseptic dressing
techniques are used to diminish the occurrence of osteomyelitis and wound
in-fections. During healing, other infections (eg, upper respiratory
infections) need to be prevented so that hematogenous spread does not result in
osteomyelitis. If the patient is receiving chemo-therapy, it is important to
monitor the white blood cell count and to instruct the patient to avoid contact
with people who have colds or other infections.
Hypercalcemia
Hypercalcemia is a dangerous complication of bone cancer.
The symptoms must be recognized and treatment initiated promptly. Symptoms
include muscular weakness, incoordination, anorexia, nausea and vomiting,
constipation, electrocardiographic changes (eg, shortened QT interval and ST
segment, bradycardia, heart blocks), and altered mental states (eg, confusion,
lethargy, psy-chotic behavior).
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Preparation for and coordination of continuing health
care are begun early as a multidisciplinary effort. Patient teaching ad-dresses
medication, dressing, treatment regimens, and the im-portance of physical and
occupational therapy programs. The nurse teaches weight-bearing limitations and
special handling to prevent pathologic fractures. It is important that the
patient and family know the signs and symptoms of possible complications as
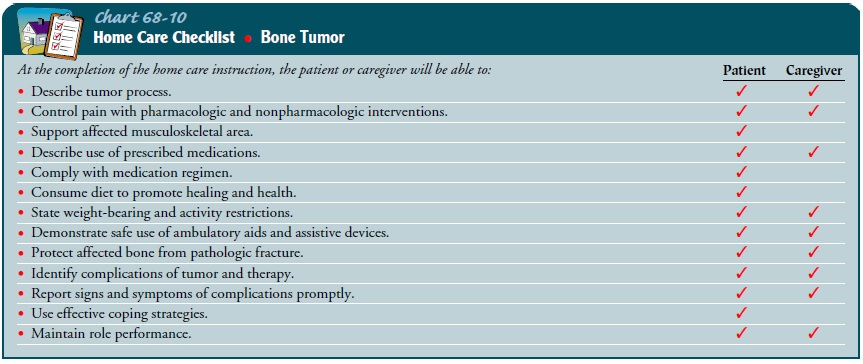
well as resources available for continuing care (Chart 68-10).
Continuing Care
Frequently, arrangements are made with a home health care agency for home care supervision and follow-up. The home care nurse as-sesses the patient’s and family’s abilities to meet the patient’s needs and determines whether the services of other agencies are needed.
The nurse advises the patient to have readily available
the tele-phone numbers of people to contact in case concerns arise.
The nurse emphasizes the need for long-term health
super-vision to ensure cure or to detect tumor recurrence or metastasis. If the
patient has metastatic disease, end-of-life issues may need to be explored.
Referral for hospice care is made if appropriate.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Describes
disease process and treatment regimen
a) Describes
pathologic condition
b) States
goals of the therapeutic regimen
c) Seeks
clarification of information
2) Achieves
control of pain
a) Uses
multiple pain control techniques, including pre-scribed medications
b) Experiences
no pain or decreased pain at rest, during ADLs, or at surgical sites
3) Experiences
no pathologic fracture
a) Avoids
stress to weakened bones
b) Uses
assistive devices safely and appropriately
c) Strengthens
uninvolved extremities with exercise
4) Demonstrates
effective coping patterns
a) Verbalizes
feelings
b) Identifies
strengths and abilities
c) Makes
decisions
d) Requests
assistance as needed
5) Demonstrates
positive self-concept
a) Identifies
home and family responsibilities that can be accomplished
b) Exhibits
confidence in own abilities
c) Demonstrates
acceptance of altered body image
d) Demonstrates
independence in ADLs
6) Exhibits
absence of complications
a) Demonstrates
wound healing
b) Experiences
no skin breakdown
c) Maintains
or increases body weight
d) Experiences
no infections
e) Does
not experience hypercalcemia
f) Manages
side effects of therapies
g) Reports
symptoms of medication toxicity or compli-cations
7) Participates
in continuing health care at home
a) Complies
with prescribed regimen (ie, takes prescribed medications, continues physical
and occupational ther-apy programs)
b) Acknowledges
need for long-term health supervision
c) Keeps
follow-up health care appointments
d) Reports
occurrence of symptoms or complications
Related Topics