Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Disorders
Nursing Process: The Patient Undergoing Surgery of the Hand or Wrist
NURSING PROCESS: THE PATIENT
UNDERGOING SURGERY OF THE HAND OR WRIST
Assessment
Surgery of the hand or wrist, unless related to major
trauma, is generally an ambulatory surgery procedure. Before surgery, the nurse
assesses the patient’s level and type of discomfort and lim-itations in
function caused by the ganglion, carpal tunnel syn-drome, Dupuytren’s
contracture, or other condition of the hand.
Nursing Diagnoses
Based on the assessment data, the nursing diagnoses for
the pa-tient undergoing surgery of the hand or wrist may include the following:
·
Risk for peripheral neurovascular
dysfunction related to sur-gical procedure
·
Acute pain related to
inflammation and swelling
·
Self-care deficit:
bathing/hygiene, dressing/grooming, feed-ing, and/or toileting related to
bandaged hands
·
Risk for infection related to
surgical procedure
Planning and Goals
The goals of the patient may include relief of pain,
improved self-care, and absence of infection.
Nursing Interventions
PROMOTING NEUROVASCULAR FUNCTION
Neurovascular assessment
of the exposed fingers every hour for the first 24 hours is essential for
monitoring function of the nerves and perfusion of the hand. The nurse compares
the af-fected hand with the unaffected hand and the postoperative sta-tus with
the documented preoperative status. The nurse asks the patient to describe the
sensations in the hands and to demonstrate finger mobility. With tendon repairs
and nerve, vascular, or skin grafts, motor function is tested only if
prescribed. The nurse as-sesses the temperature of the affected hand. Dressings
are to be supportive but nonconstrictive. Pain uncontrolled by analgesics
suggests compromised neurovascular functioning.
RELIEVING PAIN
Pain may be related to
surgery, edema, hematoma formation, or restrictive bandages. To control
swelling that may increase the pa-tient’s pain and discomfort, the nurse
elevates the hand to heart level with pillows. When higher elevation is
prescribed, an ele-vating sling may be attached to a pole used in intravenous
(IV) therapies or to an overhead frame. If the patient is ambulatory, the arm
is elevated in a conventional sling with the hand at heart level.
Intermittent ice packs to the surgical area during the
first 24 to 48 hours may be prescribed to control swelling. Unless
con-traindicated, active extension and flexion of the fingers to pro-mote
circulation are encouraged, even though movement is limited by the bulky
dressing.
Generally, the pain and discomfort can be controlled by
oral analgesics. The nurse evaluates the patient’s response to analgesics and
to other pain-control measures. Patient education concern-ing analgesics is
important.
IMPROVING SELF-CARE
During the first few
days after surgery, the patient needs assis-tance with ADLs because one hand is
bandaged and independent self-care is impaired. The patient may need to arrange
for assis-tance with feeding, bathing and hygiene, dressing, grooming, and
toileting. Within a few days, the patient develops skills in one-handed ADLs
and is usually able to function with minimal assis-tance and use of assistive
devices. The nurse encourages use of the involved hand, unless contraindicated,
within the limits of dis-comfort. As rehabilitation progresses, the patient
resumes use of the injured hand. Physical or occupational therapy–directed
ex-ercises may be prescribed. The nurse emphasizes adherence to the therapeutic
regimen.
PREVENTING INFECTION
As with all surgery, there is a risk for infection. The
nurse teaches the patient to monitor temperature and signs and symptoms that
suggest an infection. It also is important to instruct the patient to keep the
dressing clean and dry and to report any drainage, foul odor, or increased pain
and swelling. Patient education includes aseptic wound care as well as
education related to prescribed pro-phylactic antibiotics.
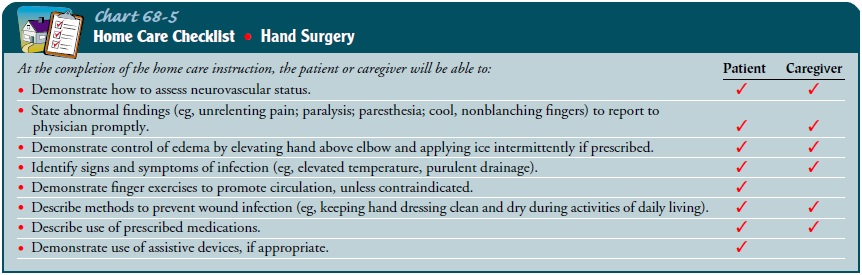
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
After the patient has undergone hand surgery, the nurse
teaches the patient how to monitor neurovascular status and the signs of
complications that need to be reported to the surgeon (eg, pares-thesia,
paralysis, uncontrolled pain, coolness of fingers, extreme swelling, excessive
bleeding, purulent drainage, fever). The nurse discusses prescribed medications
with the patient. In addition, the nurse teaches the patient to elevate the
hand above the elbow and to apply ice (if prescribed) to control swelling.
Unless con-traindicated, the nurse encourages extension and flexion exercises
of the fingers to promote circulation. The use of assistive devices is
encouraged if they would be helpful in promoting accomplish-ment of ADLs. For
bathing, the nurse instructs the patient to keep the dressing dry by covering
it with a secured plastic bag. Generally, the wound is not redressed until the
patient’s follow-up visit with the surgeon (Chart 68-5).
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Maintains
peripheral tissue perfusion
a) Demonstrates
normal skin temperature and capillary refill
b) Exhibits
normal sensations
c) Exhibits
acceptable motor function
2) Achieves
pain relief
a) Reports
increased comfort
b) Controls
edema through elevation of the hand
c) Experiences
no discomfort with movement
3) Demonstrates
independent self-care
a) Secures
assistance with ADLs during first few days post-operatively
b) Adapts
to one-handed ADLs
c) Uses
injured hand within its functional capability
4) Demonstrates
absence of wound infection
a) Complies
with treatment protocol and prevention strategies
b) Reports
temperature and pulse within normal limits
c) Experiences
no purulent wound drainage
d) Experiences
no wound inflammation
Related Topics