Chapter: Basic & Clinical Pharmacology : Drugs Used in Disorders of Coagulation
Mechanisms of Blood Coagulation
MECHANISMS OF BLOOD COAGULATION
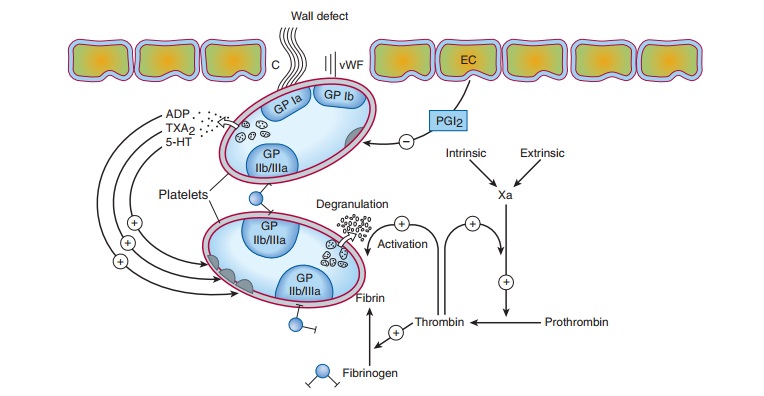
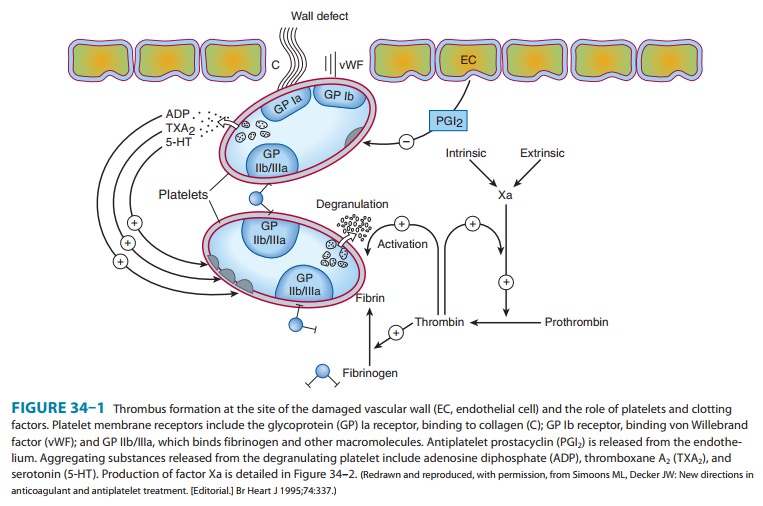
The
vascular endothelial cell layer lining blood vessels has an anti-coagulant
phenotype, and circulating blood platelets and clotting factors do not normally
adhere to it to an appreciable extent. In the setting of vascular injury, the
endothelial cell layer rapidly under-goes a series of changes resulting in a
more procoagulant pheno-type. Injury exposes reactive subendothelial matrix
proteins such as collagen and von Willebrand factor, which results in platelet
adher-ence and activation, and secretion and synthesis of vasoconstrictors and
platelet-recruiting and activating molecules. Thus, thromboxaneA2 (TXA2) is
synthesized from arachidonic acid within plateletsand is a platelet activator
and potent vasoconstrictor. Products secreted from platelet granules include adenosine diphosphate(ADP), a powerful
inducer of platelet aggregation, and
serotonin (5-HT), which stimulates aggregation and
vasoconstriction.Activation of platelets results in a conformational change in
the αIIbβIIIintegrin
(IIb/IIIa) receptor, enabling it to bind fibrinogen,which cross-links adjacent
platelets, resulting in aggregation and formation of a platelet plug (Figure
34–1). Simultaneously, the coagulation system cascade is activated, resulting
in thrombin gen-eration and a fibrin clot, which stabilizes the platelet plug .
Knowledge of the hemostatic mechanism is important for diagnosis of bleeding
disorders. Patients with defects in the forma-tion of the primary platelet plug
(defects in primary hemostasis, eg, platelet function defects, von Willebrand
disease) typically bleed from surface sites (gingiva, skin, heavy menses) with
injury. In contrast, patients with defects in the clotting mechanism
(second-ary hemostasis, eg, hemophilia A) tend to bleed into deep tissues
(joints, muscle, retroperitoneum), often with no apparent inciting event, and
bleeding may recur unpredictably.
Platelet-rich
thrombi (white thrombi) form in the
high flow rate and high shear force environment of arteries. Occlusive arterial
thrombi cause serious disease by producing downstream ischemia of extremities
or vital organs, and can result in limb
amputation or organ
failure. Venous clots tend to be more fibrin-rich, contain large numbers of
trapped red blood cells, and are recognized pathologically as red thrombi. Venous thrombi can cause
severe swelling and pain of the affected extremity, but the most feared
consequence is pulmonary embolism. This occurs when part or all of the clot
breaks off from its location in the deep venous system and travels as an
embolus through the right side of the heart and into the pulmonary arterial
circulation. Sudden occlusion of a large pulmonary artery can cause acute right
heart failure and sudden death. In addition lung ischemia or infarction will
occur distal to the occluded pulmonary arterial segment. Such emboli usually
arise from the deep venous system of the proximal lower extremities or pelvis.
Although all thrombi are mixed, the platelet nidus dominates the arterial
thrombus and the fibrin tail dominates the venous thrombus.
Related Topics