Chapter: Essentials of Psychiatry: Listening to the Patient
Listening: The Key Skill in Psychiatry
Listening:
The Key Skill in Psychiatry
It was Freud who raised the psychiatric technique
of examination – listening – to a level of expertise unexplored in earlier
eras. As Binswanger (1963) has said of the period prior to Freudian influ-ence:
psychiatric “auscultation” and “percussion” of the patient was performed as if
through the patient’s shirt with so much of his essence remaining covered or
muffled that layers of meaning remained unpeeled away or unexamined.
This metaphor and parallel to the cardiac
examination is one worth considering as we first ask if listening will remain
as central a part of psychiatric examination as in the past. The explosion of
biomedical knowledge has radically altered our evolving view and practice of
the doctor–patient relationship. Physicians of an earlier generation were
taught that the diagnosis is made at the bedside – that is, the history and
physical exami-nation are paramount. Laboratory and imaging (radiological, in
those days) examinations were seen as confirmatory exercises. However, as our
technologies have blossomed, the bedside and/or consultation room examinations
have evolved into the method whereby the physician determines what tests to
run, and the tests are often viewed as making the diagnosis. A cardiologist
colleague expresses the opinion that, given the growing availability of
non-invasive tests – echocardiograms, for example – he is not sure this is a
bad thing (Hillis, 2001, personal communication).
So can one imagine a time in the not-too-distant
future when the psychiatrist’s task will be to identify that the patient is
psychotic and then order some benign brain imaging study which will identify
the patient’s exact disorder?
Perhaps so, but will that obviate the need for the
psychiatrist’s special kind of listening? Indeed, there are those who claim
that psychiatrists should no longer be considered experts in the doctor–
patient relationship (where expertise is derived from their unique training in
listening skills) but experts in the brain (Nestler, 1999, personal
communication). As we come truly to understand the relationship between brain
states and subtle cognitive, emotional, and interpersonal states, one could
also ask if this is a distinction that really makes a difference. On the other
hand, the psychiatrist will always be charged with finding a way to relate
effectively to those who cannot effectively relate to themselves or to oth-ers.
There is something in the treatment of individuals whose illnesses express
themselves through disturbances of thinking, feeling, perceiving and behaving
that will always demand special expertise in establishing a therapeutic
relationship – and that is dependent on special expertise in listening.
Traditionally, this kind of listening has been
called “listening with the third ear” (Reik, 1954). Other efforts to label this
difficult-to-describe process have developed other terms: the interpretive
stance, interpersonal sensitivity, the narrative perspective (McHugh and
Slavney, 1986). All psychiatrists, regardless of theoretical stance, must learn
this skill and struggle with how it is to be defined and taught. The biological
or phenomenological psychiatrist listens for subtle expressions of
symptomatology; the cognitive–behav-ioral psychiatrist listens for hidden
distortions, irrational assump-tions, or global inferences; the psychodynamic
psychiatrist listens for hints at unconscious conflicts; the behaviorist
listens for covert patterns of anxiety and stimulus associations; the family
systems psychiatrist listens for hidden family myths and structures.
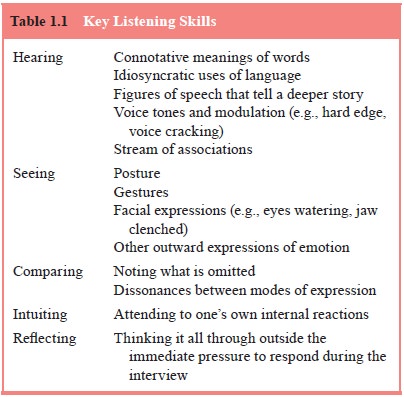
This requires sensitivity to the storyteller, which
integrates a patient orientation complementing a disease orientation. The
listener’s intent is to uncover what is wrong and to put a label on it. At the
same time, the listener is on a journey to discover who the patient is,
employing tools of asking, looking, testing and clar-ifying. The patient is
invited to collaborate as an active informer. Listening work takes time,
concentration, imagination, a sense of humor, and an attitude that places the
patient as the hero of his or her own life story. Key listening skills are
listed in Table 1.1.
The enduring art of psychiatry involves guiding the
de-pressed patient, for example, to tell his or her story of loss in addi-tion
to having him or her name, describe, and quantify symptoms
of depression. The listener, in hearing the story,
experiences the world and the patient from the patient’s point of view and
helps carry the burden of loss, lightening and transforming the load. In
hearing the sufferer, the depression itself is lifted and relieved. The
listening is healing as well as diagnostic. If done well, the listener becomes
a better disease diagnostician. The best listen-ers hear both the patient and
the disease clearly, and regard every encounter as potentially therapeutic.
Related Topics