Chapter: Essentials of Psychiatry: Law, Ethics and Psychiatry
Liability for Supervising Other Professionals
Liability for Supervising Other
Professionals
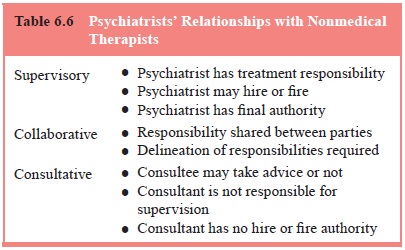
Psychiatrists work in a variety of settings and
interact in many different ways with other mental health professionals. One
as-pect of this interaction is the liability potential that psychiatrists
undertake in each of these relationships. The APA publication entitled
“Guidelines for psychiatrists in consultative, supervi-sory, or collaborative
relationships with nonmedical therapists’’ (1980) outlines the typical
consultative relationships and their corresponding degree of responsibility.
Broadly, the degree of li-ability correlates with the extent of authority to
make (as opposed to recommend) treatment decisions (Table 6.6).
Supervisory relationships are relationships in
which the psychiatrist is hierarchically and legally responsible for the
overall care of the patient, and will be held responsible for the treatment
provided by those he or she supervises. The American Psychiatric Association
(1980) guidelines state that:
In a supervisory relationship the psychiatrist
retains direct re-sponsibility for patient care and gives professional
direction and active guidance to the therapist. In this relationship the
non-medical therapist may be an employee of an organized health care setting or
of the psychiatrist. The psychiatrist remains ethi-cally and medically
responsible for the patient’s care as long as the treatment continues under his
or her supervision. The pa-tient should be fully informed of the existence and
nature of, and any changes in, the supervisory relationship.
Consultative relationships are different in terms of the level of responsibility and liability undertaken. Consultative ad-vice is given on a “take it or leave it’’ basis. Consultants are out-side the decision-making chain of command; they do not make treatment decisions, and do not have hiring and firing authority. As such, they generally are not held liable for treatment deci-sions (though psychiatrists practicing as consultants should be aware of any unusual legal provisions in the state in which they practice). The American Psychiatric Association (1980) guide-lines state that in this type of relationship the psychiatrist does not assume responsibility for the patient’s care. The psychiatrist evaluates the information provided by the therapist and offers a medical opinion which the therapist may or may not accept. Con-sultation is not a one-way process and psychiatrists do and should seek appropriate consultation from members of other disciplines in order to provide more comprehensive services to patients.
Risk Management Techniques
There is consensus among risk management experts
that various strategies can reduce medico–legal liability. The clinical
strate-gies of obtaining consultation on difficult cases, documenting the
rationale behind critical decisions, and using informed consent to build
rapport are valuable risk management techniques. In docu-mentation, “thinking
for the record’’ is advocated by Gutheil. The psychiatrist thus demonstrates
the use of judgment and ongoing risk benefit assessments. Institutional
strategies include regular quality assurance monitoring, training in
documentation, a sys-tem for working with patients and families on adverse
effects, and providing access to expert consultation.
In psychiatry, several areas deserve special
mention. Sui-cide and attempted suicide represent one of the most common and
expensive sources of lawsuits in psychiatry (Slawson, 1989). Psychiatrists
should assess the level of suicidality and the ability of patients to monitor
and report their suicidality (Gutheil et
al., 1986) and plan an appropriate strategy based on that assessment. In
lawsuits involving suicide, the patients are more commonly portrayed as the
victims, rather than agents in their own deaths. The psychiatrist who both
fosters and documents active col-laboration with the patient demonstrates good
risk management practice as well as clinical skill. Prescribing medications
also raises psychiatrists’ liability risk. Solid documentation of his-tory,
examinations, laboratory tests, indications for a medication and risk
assessment are essential to reduce liability. Consultation with a colleague
should be sought for difficult cases.
Duty to Warn, Duty to Protect
When a psychotherapist determines (or, pursuant to
the stand-ards of the profession, should determine) that his/her patient
represents a serious danger of violence to another, he/she incurs an obligation
to use reasonable care to protect the intended vic-tim against such danger. The
discharge of such duty, depending on the nature of the case, may call for the
therapist to warn the intended victim or others likely to appraise the victim
of the danger, to notify the police, or to take whatever other steps are
reasonably necessary under the circumstances.
This is the so-called Tarasoff principle,
established by California Judge Tobrinen in 1976 in the case of Tarasoff v. Regents (1976). It has generated controversy, spawned lawsuits, and initiated a fundamental
reexamination of the psychiatrist’s role vis-à-vis
members of the public.
The Tarasoff
case involved the tragic death of a Univer-sity of California student, Tatiana
Tarasoff, who was murdered by a fellow student, Prosenjit Poddar. Poddar was an
outpatient at the campus mental health clinic. He stated to his psycholo-gist
that he intended to kill Tarasoff. The therapist completedpaperwork to have
Poddar committed for 72-hour emergency psychiatric detention. The local police
detained Poddar, but re-leased him when he stated that he would “stay away from
that girl’’. Two months later he successfully carried out his threat to kill
Tarasoff.
This case, as well as subsequent cases and
legislation in other states, created new clinical and ethical dilemmas for
psy-chiatrists, as they now must balance confidentiality with the safety of
third parties in outpatient settings as well. At what point is the inherently
trusting nature of the psychiatrist–patient relationship impaired by the
legally driven obligation to report threats of harm? When should a psychiatrist
report a patient’s vague statement wishing to harm a third party? How should
the patient’s violent history be weighed in the assessment of whether to
violate confidentiality? Does the circle of responsibility in-clude only named
third parties, or does it extend to groups of reasonably identifiable potential
victims? Is a warning sufficient? Although these questions are ultimately
matters of clinical judg-ment, psychiatrists need to know whether their states
have estab-lished specific guidelines for settling them.
Related Topics