Chapter: Essentials of Psychiatry: Law, Ethics and Psychiatry
Competence, Capacity and Guardianship
Competence, Capacity and
Guardianship
Competence is best understood as a legal term
referring to an individual’s capacity to make informed decisions. Adult
indi-viduals are presumed to be legally competent, unless and until there is a
court finding of incompetence. A finding of incom-petence means that a physical
or mental illness has caused a defect in cognition or judgment, regarding the
specific area in question, such that the individual lacks the capacity to make
in-formed decisions. When a court determines that an individual is incompetent,
a guardian may be appointed to make decisions for that person.
Competence is often used as a general term, but it
should be defined specifically. With the advent of modern psychophar-macology,
competence in severely mentally ill patients is often related to medication
compliance. Even floridly psychotic pa-tients may become competent after they
are stabilized on medi-cations. Since the legal decision-making for incompetent
patients often involves determining what the individual would want if he or she
were competent to choose, it is important that the psychia-trist assess the
person’s capacity when he/she is doing clinically well, in addition to when he/she
is doing poorly.
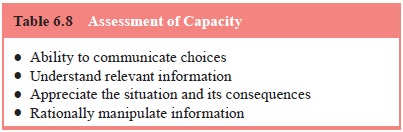
Assessing a patient’s capacity to give consent is
based on several general principles (Appelbaum and Grisso, 1988). The patient
must be able to 1) communicate choices, 2) under-stand the relevant
information, 3) appreciate the situation and its consequences, and 4)
manipulate the information rationally (Table 6.8).
There is general agreement that the standard for
judging competence also varies with the presented task. For instance the
standard for competence to consent to take an experimental drug is higher than
for taking an aspirin. The greater the risk in the
intervention, the more the psychiatrist needs to be
clear about the four elements noted in the preceding paragraph.
Several other competencies require attention in
civil mat-ters. For example, testamentary capacity (the capacity to make a
will) may be challenged by disgruntled and disinherited par-ties. For this
reason, some people obtain an evaluation of their capacity to make a will
before their death. Testamentary capacity requires that individuals understand
1) the nature of a will, 2) the extent of their assets, 3) the identity of
their natural heirs, and 4) that they should not be under undue influence.
Decision-making can be based on either the “best interests’’ standard or the
“substituted judgment’’ model. The best interests model is a paternalistic
approach that assumes that decision-makers know what is in the patient’s best
interests, and that they will act ac-cordingly. It is a value laden paradigm
that requires guardians to be aware of their own value systems, and to be on
guard against the risk that their values may conflict with those that might
apply to the patient. Perhaps more onerous, but more individualized, is the
substituted judgment model, discussed briefly above in the section on informed
consent. Here, the guardian attempts to act in the manner the person would want
under the circumstances. This is a difficult task. When an individual has never
considered a possibility, such as being in a coma, it cannot be known with
certainty what the individual’s wishes would be. While it might be generally
agreed that individualized decision-making is a preferable model, it is easy to
see why the relative comfort of the best interest approach makes this model the
one that is most widely applied.
Related Topics