Chapter: Essentials of Psychiatry: Law, Ethics and Psychiatry
Exceptions to Informed Consent
Exceptions to Informed Consent
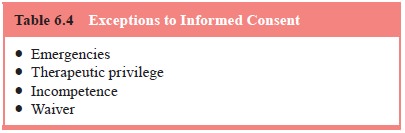
There are four primary exceptions to the general
rule that the pa-tient receiving treatment must give informed consent (Table
6.4). The first is a medical emergency. Consent is presumed when a person is
suffering from an emergent situation that requires treat-ment, but is unable to
give consent. Thus, for example, when a di-
abetic patient is in a coma and consent cannot be
obtained before giving the patient insulin, the treating physician may rely on
pre-sumed consent for treatment as a defense to a claim of battery. In
psychiatry, the definition of an emergency has been somewhat more ambiguous.
Because there is no national standard of what constitutes a psychiatric
emergency, clinicians should know the definitions (if any) in their state. They
should consider how emergent the situation is, document their assessment, and
note that it was not possible to gain the patient’s informed consent at the
time. Intervention in a psychiatric emergency, especially administration of
medication, is often not considered treatment in the same sense as emergency
treatment of a traditional medical condition. It is for this reason that many
states regulate adminis-tration of emergency psychiatric medications as
restraint, rather than as treatment.
Incompetence is the second exception to the need to
ob-tain informed consent from a patient. An incompetent person, by definition,
is incapable of giving informed consent; it can be granted only by that
person’s guardian, or other entity charged under state law with the authority
to give consent. (It is thus not truly an exception to the need for informed
consent, but a situa-tion in which the consent is obtained from a surrogate.)
Even in-competent patients should be engaged in the making of treatment
decisions, to the extent of their ability, and gaining their assent to
treatment is important, even if they do not have the legal capacity to render
informed consent. All states have procedures by which a person can be declared
incompetent; such a declaration usually requires a judicial finding, though
some states have administra-tive proceedings for resolving treatment issues
that do not require judicial intervention.
The third exception to informed consent arises from
the concept of therapeutic privilege. Psychiatrists use privilege when they
withhold information in the belief that giving a patient all of the information
necessary to make a decision would harm the patient. Invocation of therapeutic
privilege, rare in medicine, is even rarer in psychiatry, in which sharing
information is central to the work of the psychiatrist. Psychiatrists should
use this ex-ception to the informed consent doctrine exceedingly sparingly,
with extreme caution, and with great thought; here, the psychia-trist is taking
a maximally paternalistic posture in presuming what is not useful for a patient
to know. The psychiatrist assumes a grave risk of liability if the patient
suffers harm, and subse-quently proves that a reasonable patient would have
wanted to have the withheld information in order to make an informed choice
about treatment.
Waiver is the fourth exception in the informed
consent doctrine. Competent patients may request that their physicians not give
them information, effectively waiving their right to know. This circumstance
has become increasingly unusual over time as physicians are less likely to
withhold this information and patients less likely to request such a waiver.
Consent to the Treatment of Minors
Minors are considered to be incompetent for almost
all purposes, including the right to make medical decisions. Each state has its
own definition of the age that minors must attain to consent to different
treatments, and the age requirements may vary with the type of treatment. For instance,
a state may have a lower age of consent for treatment of sexually transmitted
diseases or mental illness than for traditional medical treatment.
Psychiatrists must become familiar with the law of the state or states in which
they practice.
Psychiatrists who work in schools must obtain the
consent of parents before initiating ongoing treatment. An emergency evaluation
of a student – performed without such consent – is permissible for the most
part under the doctrine of emergencies and must be documented as such (see
earlier discussion). Psychi-atrists who work in school settings also have to
work with parents who are separated or divorced. Psychiatrists are obligated to
de-termine which parent has legal custody and to obtain the consent of that parent
for the treatment of the child; documented proof of custody must be obtained.
Most states have laws by which minors may become emancipated, and therefore are
deemed competent to make their own decisions. The conditions of emancipation
typically include marriage, becoming a parent, entry into the armed services,
and sometimes a demonstrated ability of a minor to manage his or her own
financial affairs and to live on his or her own.
Related Topics