Chapter: Essentials of Psychiatry: Law, Ethics and Psychiatry
Confidentiality and Privilege
Confidentiality and Privilege
The principles of confidentiality and privilege
have a long and still evolving historical connection with the practice of
medicine and the role of the physician. The Hippocratic Oath states, “And about
whatever I may see or hear in treatment, or even without treatment, in the life
of human beings – things that should not ever be blurted out outside – I will
remain silent, holding such things to be unutterable [sacred, not to be
divulged]’’ (Von Staden, 1996). The elegant simplicity of this statement of principle
is now pitted against conflicting legal demands and societal values. The Tarasoff case (discussed below) and its
progeny, the increas-ing use of subpoenas for psychiatric records, the
complexity of interfacing with managed care, and confidentiality guidelines
related to human immunodeficiency virus infection (HIV) are just some of the
issues that complicate the psychiatrists’ oath of confidentiality.
Confidentiality
In the APA’s Principles
of Medical Ethics with Annotations Es-pecially Applicable to Psychiatry (1993),
Section 4, Annotation 1 reads,
“Confidentiality is essential to psychiatric treatment. This is based in part
on the special nature of psychiatric therapy as well as on the traditional
ethical relationship between physician and patient’’.
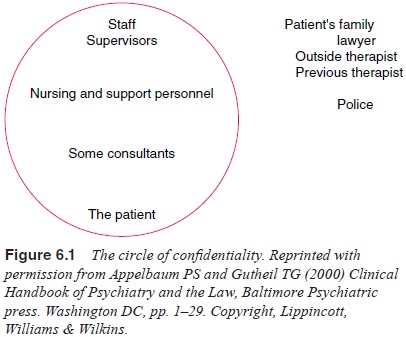
Appelbaum and Gutheil (2000) looked at practice in
psy-chiatric facilities, and devised the concept of a “circle of
confi-dentiality’’ (Figure 6.1). Within the circle, information about the
patient is shared without the patient’s consent. For instance, for a
hospitalized patient, the resident psychiatrist, the psychiatrist’s supervisor,
the staff and essential consultants are considered to be within the circle of
confidentiality. The patient’s family, the patient’s attorney, the patient’s
outside psychiatrist, the patient’s previous psychiatrist and the police are
outside the circle. As Appelbaum and Gutheil note, although the patient is
inside the circle, the patient may speak to anyone outside the circle without
restriction.
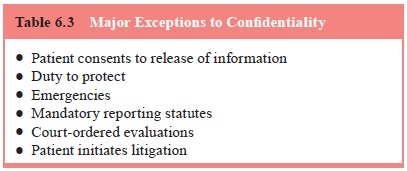
The duty of confidentiality is sometimes understood
in terms of the treatment contract between the patient and psy-chiatrist. There
is agreement between the legal system and the psychiatric profession that
confidentiality is not an absolute value. There are several major exceptions to
the obligation of
confidentiality, the most common of which is when
the patient consents to information being released. Psychiatrists and their
patients should be aware of the implications of releasing infor-mation to
insurance companies, family members, employers and so forth and should work
collaboratively in making these deci-sions (Table 6.3).
As a rule, the psychiatrist should get the
patient’s consent in writing and, optimally, the patient should read any
information that leaves the office before it is released.
The second exception is based on the duty to
protect, wherein the value of safety is given priority over the value of
confidentiality.
The third set of exceptions includes reporting
statutes, which mandate physician reporting of certain conditions. All states
have such laws in one form or another, and generally in-clude incidents of
infectious diseases, child abuse and elder abuse. If they are following any of
these statutes in good faith, psychiatrists run little risk of liability. See
the discussion of child abuse reporting, below.
The fourth set of exceptions includes emergencies.
For instance, when a psychiatrist is evaluating a patient in an emer-gency
department and the patient is grossly psychotic and unwill-ing to participate
in the interview, the psychiatrist is presented with the dilemma of whether to
contact family members or prior treaters without the expressed written consent
of the patient. This involves a risk–benefit assessment that the evaluating
psychiatrist must make. Psychiatrists must be aware of their states’ standards
concerning emergency breach of confidentiality; one state may require an
identifiable harm to be prevented, while another may permit breach when it is
necessary in the clinician’s judgment to gather the relevant information to
make a proper diagnosis or disposition for the patient.
Medical insurance has brought its own challenges to
the is-sue of confidentiality. Insurance companies may ask mental health
providers to sign a contract agreeing to release information to the insurer.
Patients may ultimately have to decide which they value more: their privacy or
the benefits obtained through the managed health company. Mental health
providers who are negotiating con-tracts with insurers should be mindful of any
obligation to provide confidential information without the patient’s consent.
Appelbaum and Gutheil (1991) state that
psychiatrists in the position of having to breach confidentiality should
observe certain basic principles. First, they should alert patients, whenever
pos-sible, of their intention to breach confidentiality before doing so.
Secondly, psychiatrists should use a hierarchy of confidentiality. Psychiatrists
do not need to jump to breach confidentiality in all situations where it is
necessary to communicate confidential in-formation. They often have time to
discuss issues with a patient, to consider alternatives and thus avoid such
confrontations. Finally, Appelbaum and Gutheil state that psychiatrists should
bear in mind that the alliance is based on the “healthy side’’ of the patient
against the patient’s illness. They suggested that when the patient is
expe-riencing impulses to harm another person, the psychiatrist and the patient
should attempt to make the call to warn the person together. The healthy side
of the patient is thus supported actively by the psy-chiatrist, as opposed to
having the psychiatrist “blow the whistle’’ on a patient who has become dangerous.
These recommendations emphasize the importance of the therapeutic alliance and
remind us that confidentiality is an important aspect of that alliance.
Psychiatrist–Patient Privilege
Privilege is defined as the patient’s right to
prevent testimony by a psychiatrist in a court setting (Gutheil, 1994;
Appelbaum and Gutheil, 1991). It rests on two primary justifications: 1) it
protects the patient’s interests in the privacy of treatment matters; and 2) it
may encourage patients to speak openly with their psychiatrists. The scope of
privilege is generally limited to the patient’s com-munications with the
psychiatrist. Observations of the patient’s demeanor, or his or her conduct or
even words in a public setting may not be covered within the privilege.
Privilege is a right belonging to the patient and
may be waived by the patient. Although the privilege does not belong to the
psychiatrist, he or she may have a duty to assert it in legal proceedings,
unless and until one of the exceptions to privilege applies. In the absence of
a release or waiver of privilege by the patient, psychiatrists should consult
with legal counsel if they are called to testify about their communications
with a patient.
Exceptions to the doctrine of privilege vary from
state to state and include situations when a patient has introduced his or her
mental state into litigation to which the patient is a party. In some states,
privilege does not apply in competence to stand trial, or criminal
responsibility evaluations. There are often exceptions in cases of child
custody, involuntary commitment proceedings, will contests, or malpractice
claims filed by the patient against a psychiatrist. Finally, state law may vary
on the scope of the exception once it is invoked.
Related Topics