Chapter: Modern Medical Toxicology: Miscellaneous Drugs and Poisons: Gastrointestinal and Endocrinal Drugs
Insulin
Insulin
Insulin
is a hormone that facilitates the penetration of glucose and amino acids
through cell membranes of skeletal and heart muscle. Insulin was first
extracted successfully from the pancre-atic islets by a young Canadian surgeon Frederick G Banting, together with a
medical student Charles H Best, in 1921. They were helped in their quest
by JRR Macleod, a professor of
physiology, and JB Collip, a
chemist. Therefore when the Nobel prize in Medicine (Physiology) was awarded to
Banting and Macleod in 1923, there was a furore prompting Banting to share his
prize with Best, while Macleod shared his with Collip.![]()
Preparations
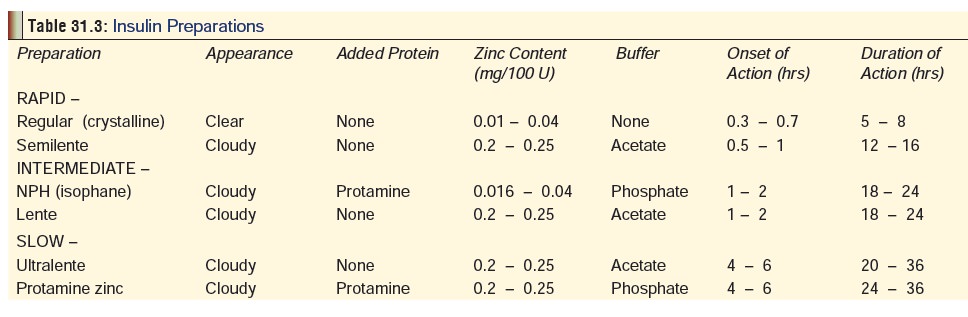
The
various preparations of insulin currently available are mentioned (along with
some relevant properties) in Table 31.3.
Uses
Subcutaneous
administration of insulin is the primary treatment for all patients with IDDM (insulin-dependant diabetes mellitus or Type I DM), and for patients with NIDDM
(non-insulin-dependant diabetes mellitus or Type II DM), that is not
adequatelycontrolled by diet or oral hypoglycaemics, and for patients with
post-pancreactectomy diabetes or gestational diabetes.
Toxicokinetics
Insulin is usually administered by
subcutaneous injection. Commercial preparations are available for either
subcutaneous or intravenous injection which differ in respect to onset and
dura-tion of action. The onset and duration of action vary considerably
depending on the preparation (Table 31.3).
Insulin is not absorbed from the GI tract. Metabolism to the extent of 50% of
the admin-istered dose occurs in the liver. The half-life of insulin is about
20 minutes if it has been injected IV, while it is 2 hours by the subcutaneous
or intramuscular route. Insulin is 5% protein bound.
Insulin is reabsorbed in the
proximal renal tubule (upto 98%), and 60% is returned to the venous blood. Less
than 2% is excreted unchanged.
Adverse Effects
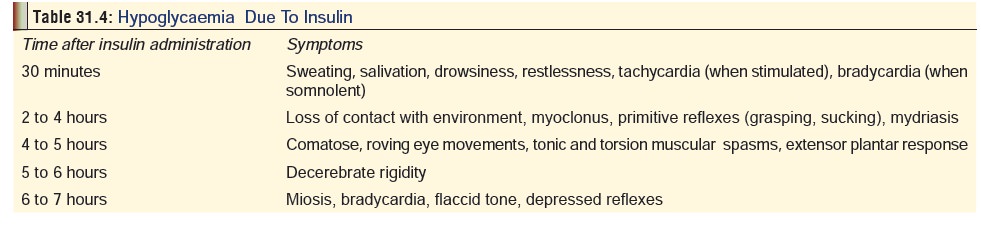
Hypoglycaemia: This remains one of the potential hazardsof insulin
therapy, and is invariably the result of inadvertent overdose. Symptoms will
depend on the extent of overdose and the time elapsed since administration (Table 31.4). Prolonged hypoglycaemia
can produce behaviour disturbances, convul-sions, coma, and death. Irreversible
neurologic sequelae are likely to occur when the duration of untreated
hypoglycaemia approaches 7 hours following overdose. Sequelae may include
amnesia, dementia, and confusion. While there is little corre-lation between
insulin dose and severity of hypoglycaemia, serious sequelae are common when
insulin is combined with other agents such as barbiturates.
Sensitivity reactions: These are more common with bovinepreparations
than with porcine insulin, while human insulin is associated with negligible
incidence of allergic reactions. Cutaneous manifestations are most common,
while in some cases there may be systemic effects. In a few cases, insulin
resistance may be encountered due to IgG antibodies.
Lipoatrophy and lipohypertrophy: The former is said to be avariant
of an immune response to insulin, while the latter is because of lipogenic
action of high local concentrations of insulin. Both are rare with purified insulin
preparations. It is advisable to rotate the site of injection frequently to
avoid these effects.
Insulin oedema: Sodium retention consequent to insulin admin-istration can result in oedema, abdominal bloating, weight gain, and blurred vision.
Drug Interactions
The
hypoglycaemic action of insulin is enhanced by fasting, alcohol, barbiturates,
salicylates, MAOIs, beta blockers, ACE inhibitors, and benzodiazepines. It is
depressed by glucagon, adrenaline, oestrogens, adrenocortical hormones, INH,
chlor-promazine and thyroxine.
Clinical (Toxic) Features
Acute Poisoning:
General—
·
Patients with intermediate or
extended insulin overdose may not develop symptoms for 18 to 36 hours except
for vomiting and lethargy. With long acting insulin, there is a compensatory
mechanism in the first 24 hours which a compensatory mechanism in the first 24
hours which helps to maintain normoglycaemia. Later this is exhausted, leading
to irreversible brain and myocardial damage due to severe hypoglycaemia.
·
After an insulin overdose, upto 12
days of treatment may be required before insulin needs return to normal.
Non-diabetic patients are found to be more likely to present with hypogly-
caemia, and develop recurrent hypoglycaemia despite oral intake and IV glucose
infusion following intentional misuse.
·
Hypoglycaemia can occur with
therapeutic doses of insulin in diabetics on an uncontrolled diet, with too
much exercise, or in patients with brittle diabetes. It is difficult to predict
the minimum toxic or lethal dose of insulin and severity of intoxication must
be based on clinical findings.
Specific—
·
Eyes: Mydriasis, sluggish external
ocular movements.
·
CNS: Drowsiness, confusion,
headache, restlessness, extensor spasms, extensor plantar reflexes, absent gag
reflex. Deep tendon reflexes may be normal, depressed or exaggerated.
Generalised seizures may accompany severe hypoglycaemia following overdose.
Aphasia, maniacal behaviour, and other personality changes secondary to
hypoglycaemia can also occur.
·
Skin: Cold, clammy, pale, with
profuse sweating.
·
Respiratory system: Breathing is
deep and heavy, with periods of apnoea. Pulmonary oedema may occur.
·
CVS: Tachycardia.
·
Extremities: Pain, cramps,
twitching.
·
Hypokalaemia may occur along with
other electrolyte abnormalities following massive insulin overdose. See also Table
31.4.
Chronic Poisoning
·
This is usually the result of
chronic overtreatment with nsulin.
·
There is recurrent, episodic
hypoglycaemia characterised by
o
Pallor, restlessness, stertorous
respiration, depression, inattentiveness.
o
Sweating.
·
Nightmares, night sweats, difficulty
in awakening.
·
Glycogen-laden hepatomegaly.
·
Morning hypothermia.
Diagnosis
·
Monitor blood sugar levels regularly. Plasma glucose levels
of 30 mg/dL or lower are common following large over-dosage. Urinary glucose
and acetone determination are also diagnostic for diabetic ketoacidosis.
Immediate differentia-tion between hypoglycaemia and ketoacidosis is accom-plished
by the use of a bedside blood glucose testing strip.
·
Plasma insulin levels do not correlate well with severity of
hypoglycaemia.
·
Leukocytosis is commonly observed.
·
Potassium levels may be depressed.
·
ECG: Sinus tachycardia, occasional
premature ventricular beats, elevated ST segments.
·
EEG: Slow diffuse waves without
lateralising discharges.
·
Urinalysis: Albuminuria, hyaline casts.
·
Chronic insulin-induced hypoglycaemia is often associated
with the presence of insulin-binding antibodies and low C-peptide levels.
Treatment
·
Stabilisation:
Airway, breathing and circulation must be estab- lished and maintained.
Endotracheal intubation and assisted ventilation may be necessary.
·
Antidote:Glucoseis the specific antidote and
must be administered without delay.
·
Give 50 ml 50% dextrose as IV bolus
upon admission.
·
Follow this up with continuous
glucose infusion of 5% or 10% dextrose in water, sufficient to maintain slight
hyperglycaemia.
·
Alternatively, if a patient is
symptomatic, or has blood glucose level <60 mg/dL administer an IV bolus (50
ml) of 50% dextrose over a period of 2 to 3 minutes. Improvement will usually
be seen in 5 to 10 minutes. A continuous IV infusion of 10 percent dextrose in
water should be started following overdosage of longer acting insulin
preparations given subcu- taneously. Monitor blood glucose levels regularly to
maintain Oral glucose cannot be relied upon to maintain eugly- caemia.
·
Glucagon
1 to 2 mg, IM, may help in mobilising hepatic glycogen
stores, but is not effective in the presence of prolonged hypoglycaemia,
fasting, or alcohol abuse. Glucagon is only effective when the patient has
adequate liver glycogen stores.
·
Adrenaline (1 : 1000), 1 mg, SC, can
be beneficial in some cases.
·
Some investigators have achieved
success by surgically excising visible injection sites down to the muscle
layer. Cerebral oedema is treated with mannitol and dexamethasone.
• Hypokalaemia is managed by potassium supplements. Administer intravenous potassium chloride (20 to 60 mEq/L of fluid) to correct cardiac arrhythmias, muscle paralysis, or EKG changes secondary to hypokalaemia.
• Administer 300 grams daily or more of carbohydrates when the patient awakens, to supplement intravenous glucose and prevent secondary hypoglycaemia.
• Excision of the skin and fat down to the muscle wall of an insulin injection site using local anaesthetic has been utilised in the management of injected insulin overdoses.
• Haemodialysis does not appear to enhance elimination of insulin.
• Permanent brain damage has been reported following injec- tion of 800 and 3200 units of insulin in diabetic patients.
• At the same time, recovery has occurred following up to 3200 units in adults.
Related Topics