Chapter: Modern Medical Toxicology: Miscellaneous Drugs and Poisons: Gastrointestinal and Endocrinal Drugs
Catecholamines
CATECHOLAMINES
The
term catecholamine refers to a
biologically active amine derived from the amino acid tyrosine. Classic
examples include adrenaline (epinephrine), and noradrenaline (norepinephrine).
Other examples include dopamine and isoproterenol, both of which have been
discussed elsewhere.
Adrenaline (Epinephrine)
Uses
·
Rapid relief of respiratory distress
due to bronchospasm.
·
Rapid relief of hypersensitivity
reactions.
·
Prolongation of action of local
anaesthetics.
·
Restoration of cardiac rhythm in
patients with cardiac arrest.
·
Topical haemostatic agent in
surgical procedures of the nose, throat and larynx.
Toxicokinetics
Adrenaline
is not effective orally since it is rapidly conjugated and oxidised in the GI
mucosa and liver. The usual route of administration is subcutaneous injection
(slow, steady absorp-tion), but it can also be given intramuscularly,
intravenously (rapid infusion can be dangerous), or by inhalation (nebulised),
or topical application.
Adrenaline
is quickly inactivated by the liver after absorp-tion by COMT and MAO.
Mode of Action
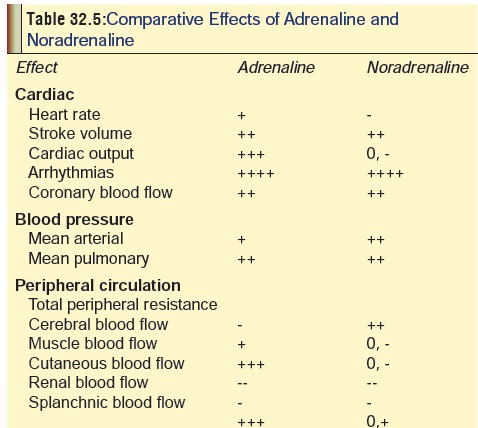
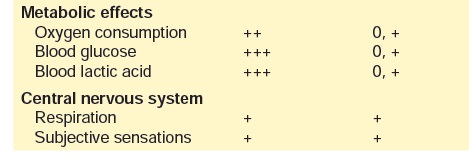
Adrenaline
is a potent stimlant of both alpha- and beta-adrenergic receptors, and
therefore has myriad effects on the body. A comparative analysis of the effects
of adrenaline and noradrenaline are mentioned in Table 32.5.
Adverse Effect
·
Fear, anxiety, restlessness,
headache, weakness, vertigo.
·
Tremor, palpitations.
·
Respiratory difficulty.
·
Cardiac arrhythmias, subarachnoid or
cerebral haemorrhage (due to rapid IV injection, or infusion of excessive
dose).
Drug Interactions
·
Accidental intra-arterial injection
of adrenaline can lead to hypotension, loss of consciousness, ventricular
tachycardia, and marked pallor of the limb. Treatment involves imme- diate
arterial injection of phentolamine (1.5 mg).
·
Rapidly acting vasodilators (sodium
nitroprusside or nitrites), and a-adrenergic blockers counteract the pressor
effects of adrenaline.
·
Use of adrenaline during anaesthesia
with halogenated hydrocarbon anaesthetics can precipitate ventricular
fibril-lation.
·
Possibility of severe hypertension and
cerebral haemor-rhage is greatly increased when adrenaline is combined with
beta-adrenergic blockers.
Clinical (Toxic) Features
·
Immediate—pallor, cyanosis, throbbing
headache, sweating,tachycardia, hypertension, chest pain, palpitations,
paraes-thesias of hands and feet, abdominal pain, and ECG changes : premature
ventricular contractions, bigeminal rhythmic changes.
·
Delayed—hypotension, metabolic acidosis,
pulmonaryoedema.
·
Accidental intra-arterial injection of adrenaline can lead
to hypotension, loss of consciousness, ventricular tachycardia, and marked
pallor of the limb. Treatment involves imme-diate arterial injection of
phentolamine (1.5 mg).
Noradrenaline (Norepinephrine, Levarterenol)
Noradrenaline
is commonly used in the treatment of shock and hypotension (especially
resulting during spinal anaesthesia, or due to overdose with
antihypertensives). Adverse effects are similar to those of adrenaline, but are
less frequent and less pronounced. Common effects include anxiety, respiratory
diffi-culty, headache, and a slow, forceful heartbeat. Overdose causes severe
hypertension with agonising headache, photophobia, stabbing chest pain, pallor,
profuse sweating, and vomiting. Treatment is on general lines as mentioned for
adrenaline.
Related Topics