Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Spinal, Epidural & Caudal Blocks
Epidural Anesthesia
Epidural Anesthesia
Continuous epidural anesthesia is a neuraxial
technique offering a range of applicationswider than the typical
all-or-nothing, single dose spinal anesthetic. An epidural block can be
per-formed at the lumbar, thoracic, or cervical level. Sacral epidural
anesthesia is referred to as a caudalblock and is described at the end of this
chap-ter. Epidural techniques are widely used forsurgical anesthesia, obstetric
analgesia, postopera-tive pain control, and chronic pain management. Epidurals
can be used as a single shot technique or with a catheter that allows intermittent
boluses and/ or continuous infusion. The motor block can range from none to
complete. All of these variables are controlled by the choice of drug,
concentration, dos-age, and level of injection.
The epidural space surrounds the dura mater posteriorly, laterally, and
anteriorly. Nerve roots travel in this space as they exit laterally through the
foramen and course outward to become peripheral nerves. Other contents of the
lumbar epidural space include fatty connective tissue, lymphatics, and a rich
venous (Batson’s) plexus. Fluoroscopic studies have suggested the presence of
septa or connective tissue bands within the epidural space, possibly explaining
the occasional one-sided epidural block.
Epidural anesthesia is slower in onset (10–20
min) and may not be as dense as spinal anesthesia. This can be manifested as a
more pronounced differential block or a segmental block, a feature that can be
useful clinically. For example, by using rela-tively dilute concentrations of a
local anesthetic combined with an opioid, an epidural provides anal-gesia
without motor block. This is commonly employed for labor and postoperative
analgesia. Moreover, a segmental block is possible because the anesthetic can
be confined close to the level at which it was injected. A segmental block is
characterized by a well-defined band of anesthesia at certain nerve roots;
leaving nerve roots above and below
unblocked. This can be seen with a thoracic epidural that provides upper
abdominal anesthesia while sparing cervical and lumbar nerve roots.
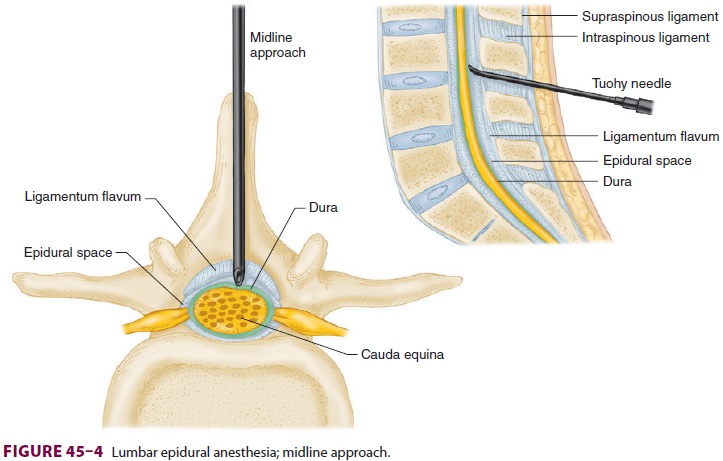
Epidural anesthesia and analgesia is most often performed in the lumbar
region. The mid-line (Figure 45–4) or paramedian approach ( Figure 45–14) can
be used. Lumbar epidural anes-thesia can be used for any procedure below the
diaphragm. Because the spinal cord typically ter-minates at the L1 level, there
is an extra measure of safety in performing the block in the lower lumbar
interspaces, particularly if an accidental dural punc-ture occurs (see
“Complications”).
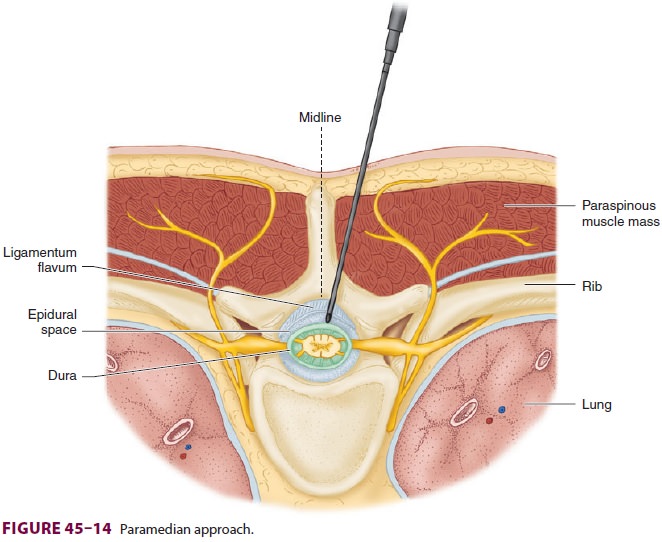
Thoracic epidural blocks are technically more difficult to accomplish
than are lumbar blocks because of greater angulation and the overlapping of the
spi-nous processes at the vertebral level (Figure 45–18).
Moreover, the potential risk of spinal cord injury with accidental dural puncture,
although exceedingly small with good technique, may be greater than that at the lumbar level. Thoracic epidural blocks can be accomplished
with either a midline or paramedian approach. Rarely used for primary
anesthesia, the thoracic epidural technique is most commonly used for
intraoperative and postoperative analgesia. Single shot or catheter techniques
are used for the manage-ment of chronic pain. Infusions via an epidural
cath-eter are useful for providing prolonged durations of analgesia and may obviate
or shorten postoperative ventilation in patients with underlying lung disease
and following chest surgery.
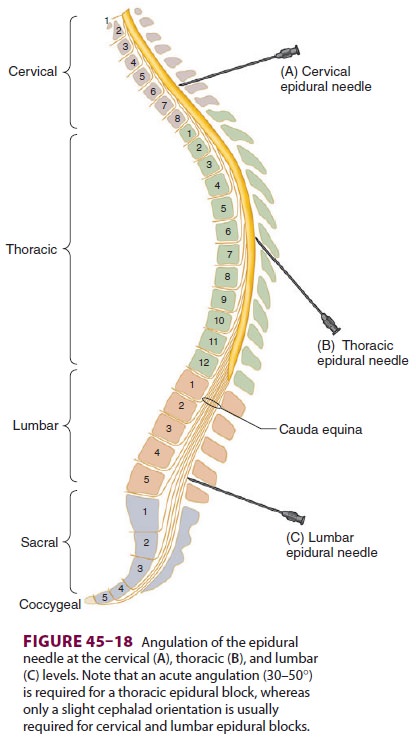
Cervical blocks are usually performed with the patient sitting, with the
neck flexed, using the mid-line approach. Clinically, they are used primarily
for the management of pain.
Related Topics