Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Spinal, Epidural & Caudal Blocks
Caudal Anesthesia

Caudal Anesthesia
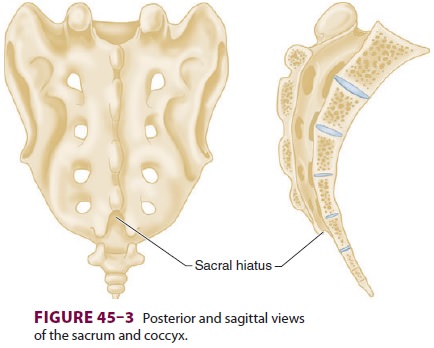
Caudal epidural
anesthesia is a
common regional technique in pediatric patients. It may also be used for
anorectal surgery in adults. The caudal space is the sacral portion of the
epidural space. Cau-dal anesthesia involves needle and/or catheter penetra-tion
of the sacrococcygeal ligament covering the sacral hiatus that is created by
the unfused S4 and S5 lami-nae. The hiatus may be felt as a groove or notch
above the coccyx and between two bony prominences, the sacral cornua (Figure
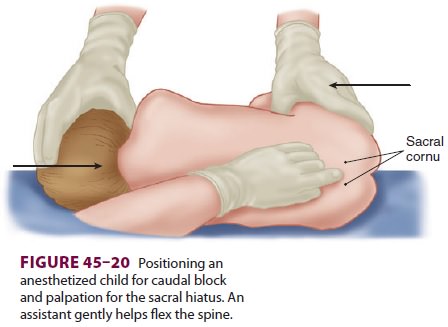
45–3). Its anatomy is more eas-ily appreciated in infants and children (Figure
45–20). The
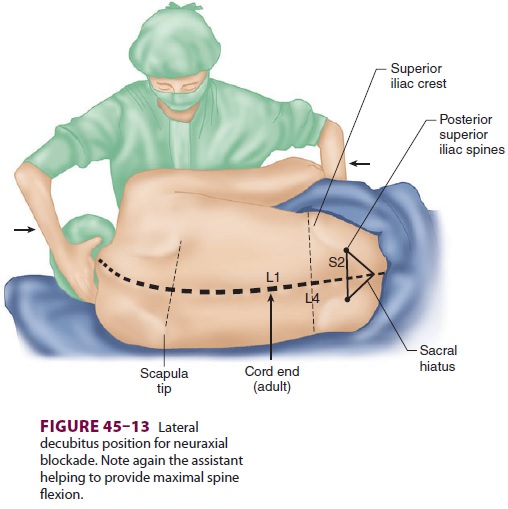
posterior superior iliac spines and the sacral hia-tus define an equilateral
triangle (Figure 45–13). Cal-cification of the sacrococcygeal ligament may make
caudal anesthesia difficult or impossible in older adults. Within the sacral
canal, the dural sac extends to the first sacral vertebra in adults and to
about the third sacral vertebra in infants, making inadvertent intrathecal
injection more common in infants.
In children, caudal anesthesia is typically
com-bined with general anesthesia for intraoperative supplementation and
postoperative analgesia. It is commonly used for procedures below the
dia-phragm, including urogenital, rectal, inguinal, and lower extremity
surgery. Pediatric caudal blocks are most commonly performed after the
induc-tion of general anesthesia. The patient is placed in the lateral or prone
position with one or both hips flexed, and the sacral hiatus is palpated. After
sterile skin preparation, a needle or intravenous catheter
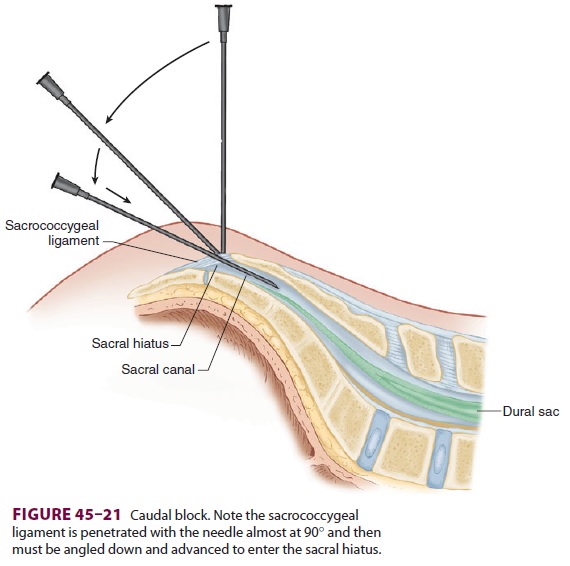
(18–23 gauge) is advanced at a 45° angle cephalad until a
pop is felt as the needle pierces the sacrococ-cygeal ligament. The angle of
the needle is then flat-tened and advanced ( Figure 45–21). Aspiration for blood and CSF is performed, and, if negative,
injec-tion can proceed. Some clinicians recommend test dosing as with other
epidural techniques, although many simply rely on incremental dosing with
fre-quent aspiration. Tachycardia (if epinephrine is used) and/or increasing
size of the T waves on elec-trocardiography may indicate intravascular
injec-tion. Clinical data have shown that the complication rate for pediatric
caudal blocks is low. Complications include total spinal and intravenous
injection, caus-ing seizure or cardiac arrest. Intraosseous injection has also
been reported to cause systemic toxicity.
A dosage of 0.5–1.0 mL/kg of 0.125–0.25%
bupivacaine (or ropivacaine), with or without epi-nephrine, can be used.
Opioids may also be added (eg, 50–70 mcg/kg of morphine), although they are not
recommended for outpatients because of the risk of delayed respiratory
depression. Addition of epinephrine will tend to increase the degree of motor
block. Clonidine is often added or substituted for local anesthetic. The
analgesic effects of the block extend for hours into the postoperative period.
Pedi-atric outpatients can safely be discharged home, even with mild residual
motor block and without urinating, as most children will urinate within 8 hr.
Repeated injections can be accomplished via
repeating the needle injection or via a catheter left in place and covered with
an occlusive dressing after being connected to extension tubing. Higher
der-matomal levels of epidural anesthesia/analgesia can be accomplished with
epidural catheters threaded cephalad into the lumbar or even thoracic epidural
space from the caudal approach in infants and chil-dren. Fluoroscopy can assist
in catheter positioning. Smaller catheters are technically difficult to pass
due to kinking. Catheters advanced into the thoracic
epidural space have been used to achieve
T2–T4 blocks for ex-premature infants undergoing inguinal hernia repair. This
is achieved using chloroprocaine (1 mL/kg) as an initial bolus and incremental
doses of 0.3 mL/kg until the desired level is achieved.
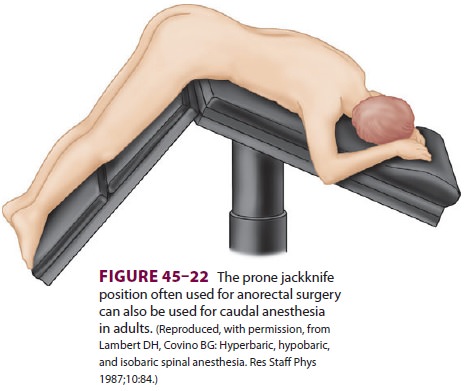
In adults undergoing anorectal procedures,
caudal anesthesia can provide dense sacral sensory blockade with limited
cephalad spread. Further-more, the injection can be given with the patient in
the prone jackknife position, which is used for surgery (Figure
45–22). A dose of 15–20 mL of 1.5–2.0% lidocaine,
with or without epinephrine, is usually effective. Fentanyl 50–100 mcg may also
be added. This technique should be avoided in patients with pilonidal cysts
because the needle may pass through the cyst track and can potentially
introduce bacteria into the caudal epidural space. Although no longer commonly
used for obstetric analgesia, a cau-dal block can be useful for the second
stage of labor, in situations in which the epidural is not reaching the sacral
nerves, or when repeated attempts at epi-dural blockade have been unsuccessful.
Related Topics