Chapter: Microbiology and Immunology: Bacteriology: Nonsporing Anaerobes
Enterobacter
Enterobacter
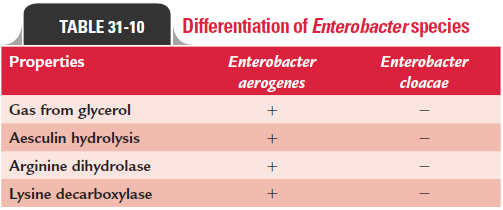
The genus Enterobacter includes 12 species, of which Enterobactercloacae and Enterobacter aerogenes, followed by Enterobacter saka-zakii are the most frequently isolated species causing humaninfections. Other species rarely associated with human infec-tions include Enterobacter asburiae, Enterobacter gergoviae, Enterobacter taylorae, and Enterobacter hormaechei. E. cloacae and E. aerogenes are two most important Enterobacter species respon-sible for a variety of nosocomial infections. Differences between E. cloacae and E. aerogenes are summarized in Table 31-10.
Enterobacter are Gram-negative bacilli, which belong to thetribe Klebsielleae, and are aerobic and facultatively anaerobic. On sheep blood agar, Enterobacter produces large, gray, and dry or mucoid colonies; on MacConkey agar, lactose-fermenting pink colonies. The bacteria ferment glucose with production of acid. They differ from Klebsiella by being motile, urease-negative, and ornithine decarboxylase-positive. Endotoxin of the bacteria is known to play a major role in the pathogenesis of sepsis and its complications.
Enterobacter species rarely cause disease in otherwise healthypeople. These are opportunistic pathogens. The patients who stay in hospital, especially in the ICU, for prolonged periods are at high risk to aquire Enterobacter infections. The patients treated earlier with antimicrobial agents and those with seri-ous underlying conditions (e.g., diabetes, malignancies, burns, mechanical ventilation), with foreign devices (e.g., such as intravenous catheters), and with immunosuppression are also at increased risk of infection by the bacteria.
In these patients, they cause frequent and severe nosoco-mial infections, such as UTIs, lower respiratory tract infections, skin and soft tissue infections, bacteremia, endocarditis, intra-abdominal infections, septic arthritis, and osteomyelitis. These infections are associated with:
· prolonged hospitalization,
· use of a variety of different surgical and nonsurgical proce-dures, and
· use of recent and expensive antimicrobial agents.
These bacteria cause significant morbidity and mortality, and infection management is complicated by multiple antibiotic resistances shown by the bacteria. These bacteria possess induc-ible beta-lactamases, which are not detectable in vitro, but are responsible for resistance during treatment. The sources of infection may be endogenous or exogenous.
· The endogenous Enterobacter infections originate from the skin, gastrointestinal tract, or urinary tract colonized by the bacteria.
· The hands of medical personnel, intravenous solutions, endoscopes, blood products, devices for monitoring intra-arterial pressure, and stethoscopes are the frequently reported sources for exogenous infections caused byEnterobacter.
Diagnosis is made by repeated culture from appropriate clini-cal specimens. Blood culture is useful in isolation of the bacte-ria from bacteremia patients.
Carbapenems, fourth-generation cephalosporins, aminogly-cosides, new quinolones, and trimethoprim–sulfamethoxazole (TMP–SMX) are the most frequently used antibiotics against Enterobacter infections.
Third-generation cephalosporins frequently show good invitro activity against these organisms, but are associated withan increased risk of developing full resistance during therapy.
Carbapenems show the best activity against E. cloacae, E. aerogenes, and other species.
First-generation and second-generation cephalosporins are not used against infections caused by Enterobacter.
Related Topics