Chapter: Basic & Clinical Pharmacology : Pharmacologic Management of Parkinsonism & Other Movement Disorders
Dopamine Receptor Agonists
DOPAMINE RECEPTOR AGONISTS
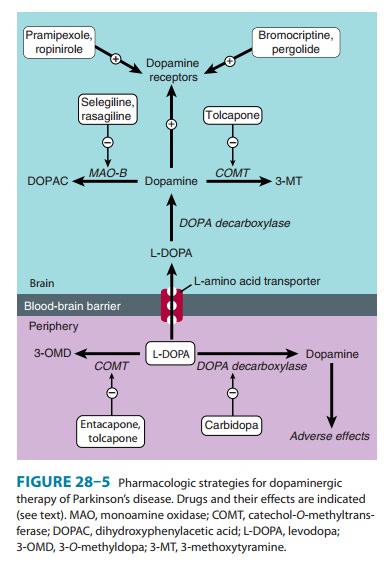
Drugs acting directly
on dopamine receptors may have a benefi-cial effect in addition to that of
levodopa (Figure 28–5). Unlike levodopa, they do not require enzymatic
conversion to an active metabolite, have no potentially toxic metabolites, and
do not compete with other substances for active transport into the blood and
across the blood-brain barrier. Moreover, drugs selec-tively affecting certain
(but not all) dopamine receptors may have more limited adverse effects than
levodopa. A number of dopamine agonists have antiparkinsonism activity. The
older dopamine agonists (bromocriptine and pergolide) are ergot (ergoline)
derivatives , and are rarely—if ever— used to treat parkinsonism. Their side
effects are of more con-cern than those of the newer agents (pramipexole and
ropinirole).
There is no evidence
that one agonist is superior to another; individual patients, however, may
respond to one but not another of these agents. Apomorphine is a potent
dopamine agonist but is discussed separately in a later section because it is
used primarily as a rescue drug for patients with disabling response
fluctuations to levodopa.
Dopamine agonists have
an important role as first-line therapy for Parkinson’s disease, and their use
is associated with a lower incidence of the response fluctuations and
dyskinesias that occur with long-term levodopa therapy. In consequence,
dopaminergic therapy may best be initiated with a dopamine agonist.
Alternatively, a low dose of carbidopa plus levodopa (eg, Sinemet-25/100 three
times daily) is introduced, and a dopamine agonist is then added. In either
case, the dose of the dopamine agonist is built up gradu-ally depending on
response and tolerance. Dopamine agonists may also be given to patients with
parkinsonism who are taking levodopa and who have end-of-dose akinesia or
on-off phenome-non or are becoming resistant to treatment with levodopa. In
such circumstances, it is generally necessary to lower the dose of levodopa to
prevent intolerable adverse effects. The response to a dopamine agonist is
generally disappointing in patients who have never responded to levodopa.
Bromocriptine
Bromocriptine is a D2 agonist; its
structure is shown in Table 16–6. This drug has been widely used to treat
Parkinson’s disease in the past but is now rarely used for this purpose, having
been super-seded by the newer dopamine agonists. The usual daily dose of
bromocriptine for parkinsonism varies between 7.5 and 30 mg. To minimize
adverse effects, the dose is built up slowly over 2 or 3 months depending on
response or the development of adverse reactions.
Pergolide
Pergolide, another
ergot derivative, directly stimulates both D1 and D2 receptors. It too has been widely used for
parkinsonism but is no longer available in the United States because its use
has been associated with the development of valvular heart disease.
Pramipexole
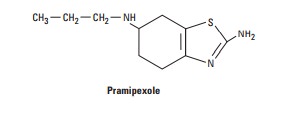
Pramipexole is not an
ergot derivative, but it has preferential affin-ity for the D3 family of receptors.
It is effective as monotherapy for mild parkinsonism and is also helpful in
patients with advanced disease, permitting the dose of levodopa to be reduced
and smoothing out response fluctuations. Pramipexole may ameliorate affective
symptoms. A possible neuroprotective effect has been suggested by its ability
to scavenge hydrogen peroxide and enhance neurotrophic activity in
mesencephalic dopaminergic cell cultures.
Pramipexole is rapidly
absorbed after oral administration, reach-ing peak plasma concentrations in
approximately 2 hours, and is excreted largely unchanged in the urine. It is
started at a dosage of 0.125 mg three times daily, doubled after 1 week, and
again after another week. Further increments in the daily dose are by 0.75 mg
at weekly intervals, depending on response and tolerance. Most patients require
between 0.5 and 1.5 mg three times daily. Renal insufficiency may necessitate
dosage adjustment. An extended-re-lease preparation is now available and is
taken once daily at a dose equivalent to the total daily dose of standard
pramipexole. The extended-release preparation is generally more convenient for
patients and avoids swings in blood levels of the drug over the day.
Ropinirole
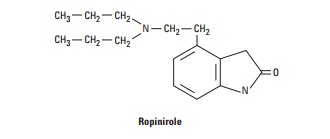
Another nonergoline
derivative, ropinirole (now available in a generic preparation) is a relatively
pure D2 receptor agonist that
is effective as monotherapy in patients with mild disease and as a means of
smoothing the response to levodopa in patients with more advanced disease and
response fluctuations. It is introduced at 0.25 mg three times daily, and the
total daily dose is then increased by 0.75 mg at weekly intervals until the
fourth week and by 1.5 mg thereafter. In most instances, a dosage between 2 and
8 mg three times daily is necessary. Ropinirole is metabolized by CYP1A2; other
drugs metabolized by this isoform may signifi-cantly reduce its clearance. A
prolonged-release preparation taken once daily is now available.
Rotigotine
The dopamine agonist
rotigotine, delivered daily through a skin patch, was approved in 2007 by the
Food and Drug Administration (FDA) for treatment of early Parkinson’s disease.
It supposedly pro-vides more continuous dopaminergic stimulation than oral
medica-tion in early disease; its efficacy in more advanced disease is less
clear. Benefits and side effects are similar to those of other dopamine
ago-nists but reactions may also occur at the application site and are
sometimes serious. The product was recalled in the United States in 2008
because of crystal formation on the patches, affecting the avail-ability and
efficacy of the agonist. It is still available in Europe.
Adverse Effects of Dopamine Agonists
A. Gastrointestinal Effects
Anorexia and nausea
and vomiting may occur when a dopamine agonist is introduced and can be
minimized by taking the medica-tion with meals. Constipation, dyspepsia, and
symptoms of reflux esophagitis may also occur. Bleeding from peptic ulceration
has been reported.
B. Cardiovascular Effects
Postural hypotension
may occur, particularly at the initiation of therapy. Painless digital
vasospasm is a dose-related complication of long-term treatment with the ergot
derivatives (bromocriptine or pergolide). When cardiac arrhythmias occur, they
are an indica-tion for discontinuing treatment. Peripheral edema is sometimes
problematic. Cardiac valvulopathy may occur with pergolide.
C. Dyskinesias
Abnormal movements
similar to those introduced by levodopa may occur and are reversed by reducing
the total dose of dopamin-ergic drugs being taken.
D. Mental Disturbances
Confusion,
hallucinations, delusions, and other psychiatric reac-tions are potential
complications of dopaminergic treatment and are more common and severe with
dopamine receptor agonists than with levodopa. Disorders of impulse control may
lead to compulsive gambling, shopping, betting, sexual activity, and other
behaviors . They clear on withdrawal of the offending medication.
E. Miscellaneous
Headache, nasal
congestion, increased arousal, pulmonary infil-trates, pleural and
retroperitoneal fibrosis, and erythromelalgia are other reported adverse
effects of the ergot-derived dopamine ago-nists. Cardiac valvulopathies have
occurred with pergolide. Erythromelalgia consists of red, tender, painful,
swollen feet and, occasionally, hands, at times associated with arthralgia;
symptoms and signs clear within a few days of withdrawal of the causal drug. In
rare instances, an uncontrollable tendency to fall asleep at inap-propriate
times has occurred, particularly in patients receiving pramipexole or ropinirole;
this requires discontinuation of the medication.
Contraindications
Dopamine agonists are
contraindicated in patients with a history of psychotic illness or recent
myocardial infarction, or with active peptic ulceration. The ergot-derived
agonists are best avoided in patients with peripheral vascular disease.
Related Topics