Chapter: Basic & Clinical Pharmacology : Histamine, Serotonin, & the Ergot Alkaloids
Clinical Pharmacology of Serotonin
CLINICAL PHARMACOLOGY OF
SEROTONIN
Serotonin Agonists
Serotonin
has no clinical applications as a drug. However, several receptor
subtype-selective agonists have proved to be of value. Buspirone, a 5-HT1Aagonist, has received wide attention
for itsusefulness as an effective nonbenzodiazepine anxiolytic . Dexfenfluramine, another selective 5-HT
agonist, was widely used as an appetite suppressant but was withdrawn because
of cardiac valve toxicity. Appetite suppression appears to be associated with
agonist action at 5-HT2C receptors in the cen-tral nervous system.
5-HT1D/1B Agonists & Migraine Headache
The
5-HT1D/1B agonists (triptans,
eg, sumatriptan) are used almost
exclusively for migraine headache. Migraine in its “classic” form is
characterized by an aura of variable duration that may involve nausea,
vomiting, visual scotomas or even hemianopsia, and speech abnormalities; the
aura is followed by a severe throb-bing unilateral headache that lasts for a
few hours to 1–2 days. “Common” migraine lacks the aura phase, but the headache
is similar. After a century of intense study, the pathophysiology of migraine
is still poorly understood and controversial. Although the symptom pattern and
duration of prodrome and headache vary markedly among patients, the severity of
migraine headache justifies vigorous therapy in the great majority of cases.
Migraine
involves the trigeminal nerve distribution to intracra-nial (and possibly
extracranial) arteries. These nerves release pep-tide neurotransmitters,
especially calcitonin gene-related
peptide (CGRP;), an extremely powerful vasodilator. Substance P and
neurokinin A may also be involved. Extravasation of plasma and plasma proteins
into the perivascular space appears to be a common feature of animal migraine
models and is found in biopsy specimens from migraine patients. This effect
probably reflects the action of the neuropeptides on the vessels. The
mechanical stretching caused by this perivascular edema may be the immediate
cause of activation of pain nerve endings in the dura. The onset of headache is
sometimes associated with a marked increase in amplitude of temporal artery
pulsations, and relief of pain by administration of effective therapy is
sometimes accompanied by diminution of the arterial pulsations.
The
mechanisms of action of drugs used in migraine are poorly understood, in part
because they include such a wide variety of drug groups and actions. In
addition to the triptans, these include ergot alkaloids, nonsteroidal anti-inflammatory
analgesic agents, β-adrenoceptor
blockers, calcium channel blockers, tricyclic anti-depressants and SSRIs, and
several antiseizure agents. Furthermore, some of these drug groups are
effective only for prophylaxis and not for the acute attack.
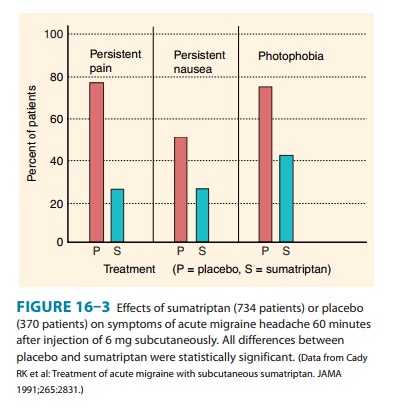
Two primary hypotheses have been proposed to explain the actions of these drugs. First, the triptans, the ergot alkaloids, and antidepressants may activate 5-HT1D/1B receptors on presynaptic trigeminal nerve endings to inhibit the release of vasodilating pep-tides, and antiseizure agents may suppress excessive firing of these nerve endings. Second, the vasoconstrictor actions of direct 5-HT agonists (the triptans and ergot) may prevent vasodilation and stretching of the pain endings. It is possible that both mechanisms contribute in the case of some drugs. Sumatriptan and its conge-ners are currently first-line therapy for acute severe migraine attacks in most patients (Figure 16–3). However, they should not be used in patients at risk for coronary artery disease. Anti-inflammatory analgesics such as aspirin and ibuprofen are often helpful in controlling the pain of migraine. Rarely, parenteral opioids may be needed in refractory cases. For patients with very severe nausea and vomiting, parenteral metoclopramide may be helpful.
Propranolol, amitriptyline, and some calcium
channel block-ers have been found to be effective for the prophylaxis of
migraine in some patients. They are of no value in the treatment of acute migraine.
The anticonvulsants valproic acid
and topiramate have also been found to have prophylactic
efficacy in many migraine patients. Flunarizine,
a calcium channel blocker used in Europe, has been reported in clinical trials
to effectively reduce the severity of the acute attack and to prevent
recurrences. Verapamil appears to
have modest efficacy as prophylaxis againstmigraine.
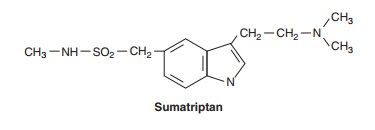
Sumatriptan
and the other triptans are selective agonists for 5-HT 1D and 5-HT1B
receptors; the similarity of the triptan struc-ture to that of the 5-HT nucleus
can be seen in the structure below. These receptor types are found in cerebral
and meningeal vessels and mediate vasoconstriction. They are also found on
neu-rons and probably function as presynaptic inhibitory receptors.
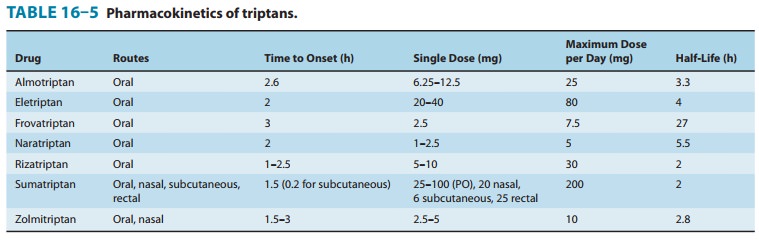
The
efficacies of all the triptan 5-HT1 agonists in migraine are equal
to each other and equivalent to or greater than those of other acute drug
treatments, eg, parenteral, oral, and rectal ergot alka-loids. The
pharmacokinetics of the triptans differ significantly and are set forth in
Table 16–5. Most adverse effects are mild and include altered sensations
(tingling, warmth, etc), dizziness, muscle weakness, neck pain, and for
parenteral sumatriptan, injection site reactions. Chest discomfort occurs in
1–5% of patients, and chest pain has been reported, probably because of the
ability of these drugs to cause coronary vasospasm. They are therefore
contraindi-cated in patients with coronary artery disease and in patients with
angina. Another disadvantage is the fact that their duration of effect
(especially that of almotriptan, sumatriptan, rizatriptan, and zolmitriptan,
Table 16–5) is often shorter than the duration of the headache. As a result, several
doses may be required during a pro-longed migraine attack, but their adverse
effects limit the maxi-mum safe daily dosage. In addition, these drugs are
expensive. Naratriptan and eletriptan are contraindicated in patients with
severe hepatic or renal impairment or peripheral vascular syn-dromes;
frovatriptan in patients with peripheral vascular disease; and zolmitriptan in
patients with Wolff-Parkinson-White syn-drome. The brand name triptans are
extremely expensive; thus generic sumatriptan should be used whenever possible.
Other Serotonin Agonists in Clinical Use
Cisapride,a 5-HT4agonist,
was used in the treatment of gastro-esophageal reflux and motility disorders.
Because of toxicity, it is now available only for compassionate use in the USA.
Tegaserod, a 5-HT4 partial agonist, is used for irritable bowel
syndrome with constipation.
Compounds such as fluoxetine and other SSRIs, which modu-late serotonergic transmission by blocking reuptake of the trans-mitter, are among the most widely prescribed drugs for the management of depression and similar disorders.
Related Topics