Chapter: Basic & Clinical Pharmacology : Histamine, Serotonin, & the Ergot Alkaloids
Clinical Pharmacology of Ergot Alkaloids
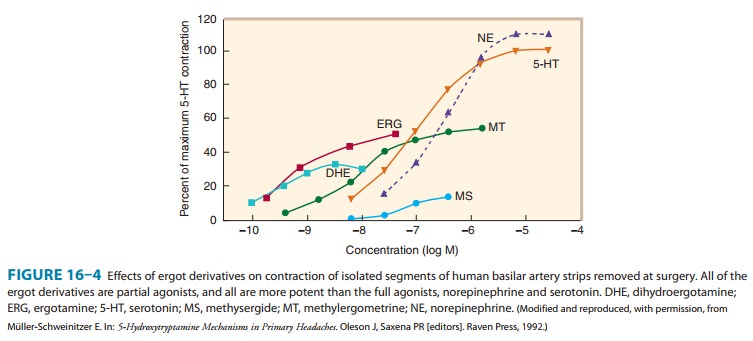
CLINICAL PHARMACOLOGY OF ERGOT
ALKALOIDS
Clinical Uses
In
spite of their significant toxicities, ergot alkaloids are still widely used in
patients with migraine headache or pituitary dysfunction, but only occasionally
in the postpartum patient.
A. Migraine
Ergot
derivatives are highly specific for migraine pain; they are not analgesic for
any other condition. Although the triptan drugs discussed above are preferred
by most clinicians and patients, tra-ditional therapy with ergotamine can also
be effective when given during the prodrome of an attack; it becomes
progressively less effective if delayed. Ergotamine tartrate is available for
oral, sub-lingual, rectal suppository, and inhaler use. It is often combined
with caffeine (100 mg caffeine for each 1 mg ergotamine tartrate) to facilitate
absorption of the ergot alkaloid.
The
vasoconstriction induced by ergotamine is long-lasting and cumulative when the
drug is taken repeatedly, as in a severe migraine attack. Therefore, patients
must be carefully informed that no more than 6 mg of the oral preparation may
be taken for each attack and no more than 10 mg per week. For very severe
attacks, ergotamine tartrate, 0.25–0.5 mg, may be given intravenously or
intramuscu-larly. Dihydroergotamine,
0.5–1 mg intravenously, is favored by some clinicians for treatment of
intractable migraine. Intranasal dihydroergotamine may also be effective.
Methysergide, which was used for
migraine prophylaxis in the past, was withdrawn because of toxicity, .
B. Hyperprolactinemia
Increased
serum levels of the anterior pituitary hormone prolactin are associated with
secreting tumors of the gland and also with the use of centrally acting
dopamine antagonists, especially the D2-blocking antipsychotic
drugs. Because of negative feedback effects, hyperprolactinemia is associated
with amenorrhea and infertility in women as well as galactorrhea in both sexes.
Rarely, the prolac-tin surge that occurs around the end of term pregnancy may
be associated with heart failure; cabergoline has been used to treat this cardiac
condition successfully.
Bromocriptine
is extremely effective in reducing the high levels of prolactin that result
from pituitary tumors and has even been associated with regression of the tumor
in some cases. The usual dosage of bromocriptine is 2.5 mg two or three times
daily. Cabergoline is similar but more potent. Bromocriptine has also been used
in the same dosage to suppress physiologic lactation. However, serious
postpartum cardiovascular toxicity has been reported in association with the
latter use of bromocriptine or pergolide, and this application is discouraged .
C. Postpartum Hemorrhage
The
uterus at term is extremely sensitive to the stimulant action of ergot, and
even moderate doses produce a prolonged and powerful spasm of the muscle quite unlike
natural labor. Therefore, ergot derivatives should be used only for control of
postpartum uterine bleeding and should never be given before delivery. Oxytocin
is the preferred agent for control of postpartum hemorrhage, but if this
peptide agent is ineffective, ergonovine maleate, 0.2 mg given intramuscularly,
can be tried. It is usually effective within 1–5 minutes and is less toxic than
other ergot derivatives for this application. It is given at the time of
delivery of the placenta or immediately afterward if bleeding is significant.
D. Diagnosis of Variant Angina
Ergonovine
given intravenously produces prompt vasoconstric-tion during coronary
angiography to diagnose variant angina if reactive segments of the coronary
arteries are present. In Europe, methylergometrine has been used for this
purpose.
E. Senile Cerebral Insufficiency
Dihydroergotoxine,
a mixture of dihydro-α-ergocryptine and three similar dihydrogenated
peptide ergot alkaloids (ergoloid mesylates), has been promoted for many years
for the relief of senility and more recently for the treatment of Alzheimer’s
demen-tia. There is no useful evidence that this drug has significant benefit.
Toxicity & Contraindications
The
most common toxic effects of the ergot derivatives are gastrointestinal
disturbances, including diarrhea, nausea, and vomiting. Activation of the
medullary vomiting center and of the gastrointestinal serotonin receptors is
involved. Since migraine attacks are often associated with these symptoms
before therapy is begun, these adverse effects are rarely contraindications to
the use of ergot.
A
more dangerous toxic effect—usually associated with over-dosage—of agents like
ergotamine and ergonovine is prolonged vasospasm. This sign of vascular smooth
muscle stimulation may result in gangrene and may require amputation. Bowel
infarction has also been reported and may require resection. Peripheral
vas-cular vasospasm caused by ergot is refractory to most vasodilators, but
infusion of large doses of nitroprusside or nitroglycerin has been successful
in some cases.
Chronic
therapy with methysergide was associated with con-nective tissue proliferation
in the retroperitoneal space, the pleural cavity, and the endocardial tissue of
the heart. These changes occurred insidiously over months and presented as
hydronephrosis (from obstruction of the ureters) or a cardiac murmur (from
dis-tortion of the valves of the heart). In some cases, valve damage required
surgical replacement. As a result, this drug was with-drawn from the US market.
Similar fibrotic change has resulted from the chronic use of 5-HT agonists
promoted in the past for weight loss (fenfluramine, dexfenfluramine).
Other
toxic effects of the ergot alkaloids include drowsiness and, in the case of
methysergide, occasional instances of central stimulation and hallucinations.
In fact, methysergide was some-times used as a substitute for LSD by members of
the so-called drug culture.
Contraindications
to the use of ergot derivatives consist of the obstructive vascular diseases,
especially symptomatic coronary artery disease, and collagen diseases.
There
is no evidence that ordinary use of ergotamine for migraine is hazardous in
pregnancy. However, most clinicians counsel restraint in the use of the ergot
derivatives by pregnant patients. Use to deliberately cause abortion is
contraindicated because the high doses required often cause dangerous
vasocon-striction.
Related Topics