Chapter: Basic & Clinical Pharmacology : Histamine, Serotonin, & the Ergot Alkaloids
Clinical Pharmacology of H1-Receptor Antagonists
CLINICAL PHARMACOLOGY OF H1-RECEPTOR
ANTAGONISTS
Clinical Uses
First-generation
H1-receptor blockers are among the most extensively promoted and
used over-the-counter drugs. The prevalence of allergic conditions and the relative safety of the drugs contribute
to this heavy use. The fact that they do cause sedation contributes to heavy prescrib-ing
and over-the-counter use of second-generation antihistamines.
A. Allergic Reactions
The
H1 antihistaminic agents are often the first drugs used to prevent
or treat the symptoms of allergic reactions. In allergic rhinitis (hay fever),
the H1 antagonists are second-line drugs after glucocorticoids
administered by nasal spray. In urticaria, in which histamine is the primary
mediator, the H1 antagonists are the drugs of choice and are often
quite effective if given before expo-sure. However, in bronchial asthma, which
involves several media-tors, the H1 antagonists are largely
ineffective.
Angioedema
may be precipitated by histamine release but appears to be maintained by
peptide kinins that are not affected by antihistaminic agents. For atopic dermatitis,
antihistaminic drugs such as diphenhydramine are used mostly for their sedative
side effect, which reduces awareness of itching.
The
H1 antihistamines used for treating allergic conditions such as hay
fever are usually selected with the goal of minimizing sedative effects; in the
USA, the drugs in widest use are the alkylamines and the second-generation
nonsedating agents. However, the sedative effect and the therapeutic efficacy
of differ-ent agents vary widely among individuals. In addition, the clinical
effectiveness of one group may diminish with continued use, and switching to
another group may restore drug effectiveness for as yet unexplained reasons.
The
second-generation H1 antagonists are used mainly for the treatment
of allergic rhinitis and chronic urticaria. Several double-blind comparisons
with older agents (eg, chlorpheniramine) indi-cated about equal therapeutic
efficacy. However, sedation and interference with safe operation of machinery,
which occur in about 50% of subjects taking first-generation antihistamines,
occurred in only about 7% of subjects taking second-generation agents. The
newer drugs are much more expensive, even in over-the-counter generic formulations.
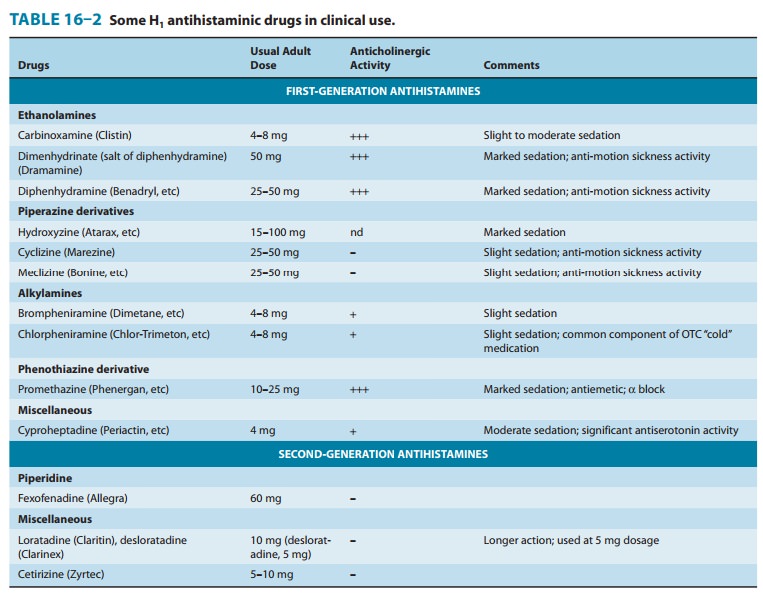
B. Motion Sickness and Vestibular Disturbances
Scopolamine and certain first-generation H1
antagonists are the most effective agents available for the preven-tion of
motion sickness. The antihistaminic drugs with the great-est effectiveness in
this application are diphenhydramine and promethazine. Dimenhydrinate, which is
promoted almost exclu-sively for the treatment of motion sickness, is a salt of
diphenhy-dramine and has similar efficacy. The piperazines (cyclizine and
meclizine) also have significant activity in preventing motion sick-ness and
are less sedating than diphenhydramine in most patients. Dosage is the same as
that recommended for allergic disorders (Table 16–2). Both scopolamine and the
H1 antagonists are more effective in preventing motion sickness when
combined with ephedrine or amphetamine.
It
has been claimed that the antihistaminic agents effective in prophylaxis of
motion sickness are also useful in Ménière’s syn-drome, but efficacy in the
latter application is not established.
C. Nausea and Vomiting of Pregnancy
Several
H1-antagonist drugs have been studied for possible use in treating
“morning sickness.” The piperazine derivatives were with-drawn from such use
when it was demonstrated that they have teratogenic effects in rodents.
Doxylamine, an ethanolamine H1 antagonist, was promoted for this
application as a component of Bendectin, a prescription medication that also
contained pyridoxine. Possible teratogenic effects of doxylamine were widely
publicizedin the lay press after 1978 as a result of a few case reports of
fetal malformation that occurred after maternal ingestion of Bendectin.
However, several large prospective studies involving over 60,000 pregnancies,
of which more than 3000 involved maternal Bendectin ingestion, disclosed no
increase in the incidence of birth defects. Nonetheless, because of the
continuing controversy, adverse publicity, and lawsuits, the manufacturer of
Bendectin withdrew the product from the market.
Toxicity
The
wide spectrum of nonantihistaminic effects of the H1 antihista-mines
is described above. Several of these effects (sedation, antimus-carinic action)
have been used for therapeutic purposes, especially in over-the-counter
remedies . Nevertheless, these two effects constitute the most common
undesirable actions when these drugs are used to block histamine receptors.
Less
common toxic effects of systemic use include excitation and convulsions in
children, postural hypotension, and allergic responses. Drug allergy is
relatively common after topical use of H1 antago-nists. The effects
of severe systemic overdosage of the older agents resemble those of atropine
overdosage and are treated in the same way. Overdosage of astemizole or
terfena-dine may induce cardiac arrhythmias; the same effect may be caused at
normal dosage by interaction with enzyme inhibitors (see Drug Interactions).
These drugs are no longer marketed in the USA.
Drug Interactions
Lethal
ventricular arrhythmias occurred in several patients taking either of the early
second-generation agents, terfenadine or astem-izole, in combination with
ketoconazole, itraconazole, or mac-rolide antibiotics such as erythromycin.
These antimicrobial drugs inhibit the metabolism of many drugs by CYP3A4 and
cause sig-nificant increases in blood concentrations of the antihistamines. The
mechanism of this toxicity involves blockade of the HERG (IKr)
potassium channels in the heart that contribute to repolariza-tion of the
action potential . The result is prolon-gation and a change in shape of the
action potential, and these changes lead to arrhythmias. Both terfenadine and
astemizole were withdrawn from the US market in recognition of these problems.
Where still available, terfenadine and astemizole should be consid-ered to be
contraindicated in patients taking ketoconazole, itra-conazole, or macrolides
and in patients with liver disease. Grapefruit juice also inhibits CYP3A4 and
has been shown to increase blood levels of terfenadine significantly.
For
those H1 antagonists that cause significant sedation, con-current
use of other drugs that cause central nervous system depression produces
additive effects and is contraindicated while driving or operating machinery.
Similarly, the autonomic blocking effects of older antihistamines are additive
with those of antimus-carinic and α-blocking drugs.
Related Topics