Chapter: Essentials of Anatomy and Physiology: Blood
White Blood Cells: Classification and Function
WHITE BLOOD CELLS
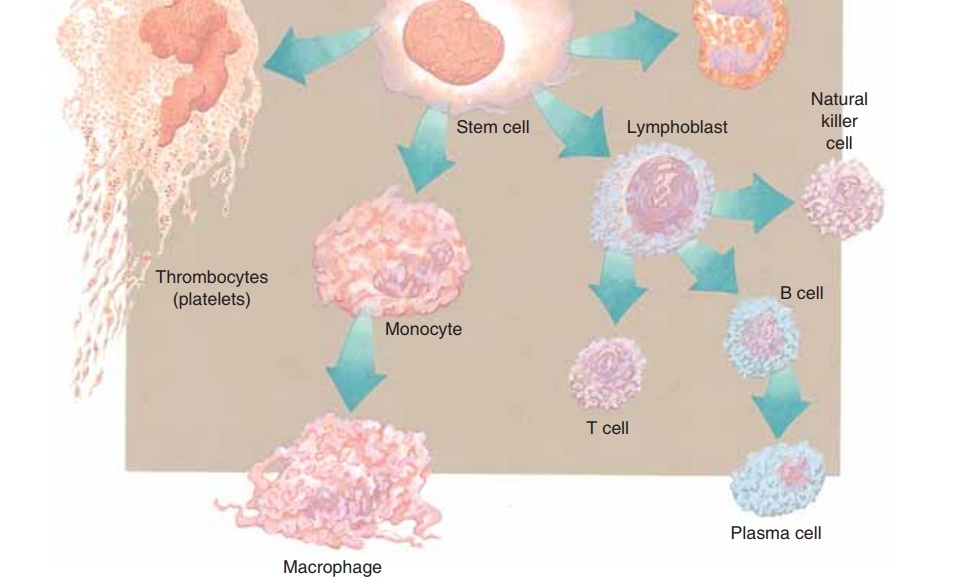
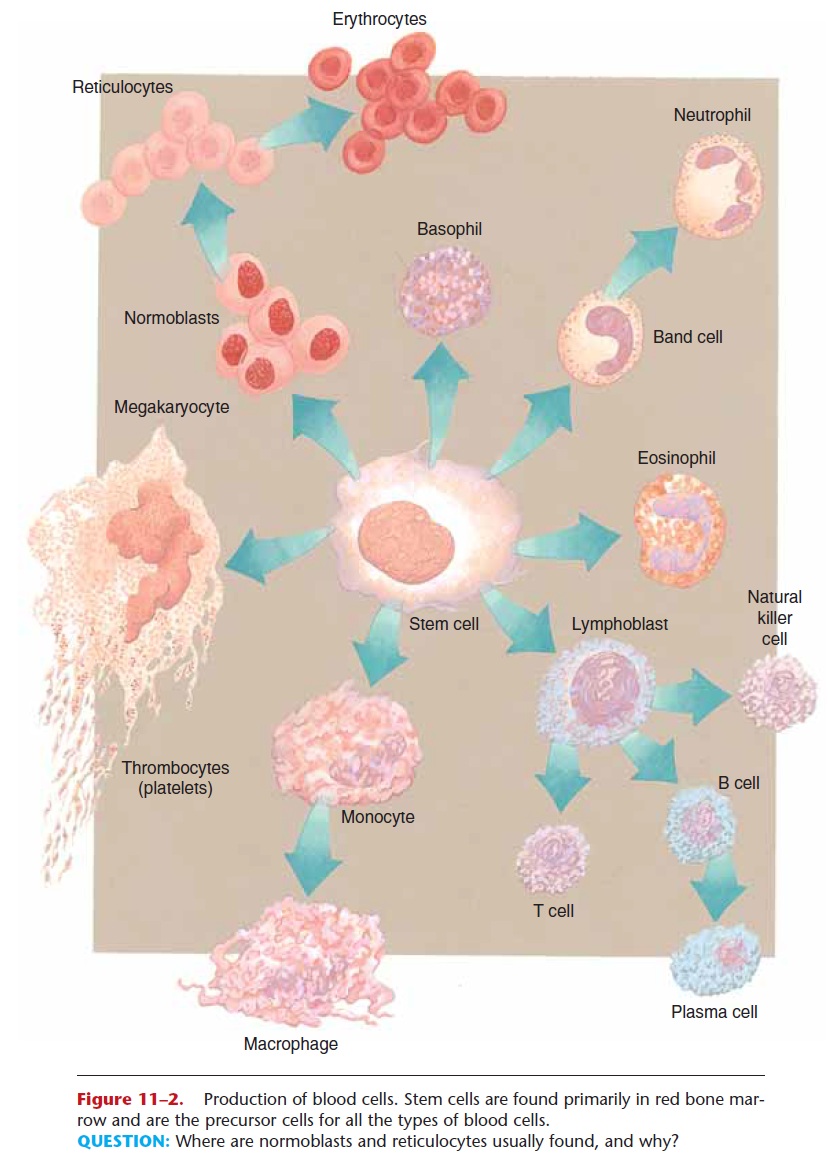
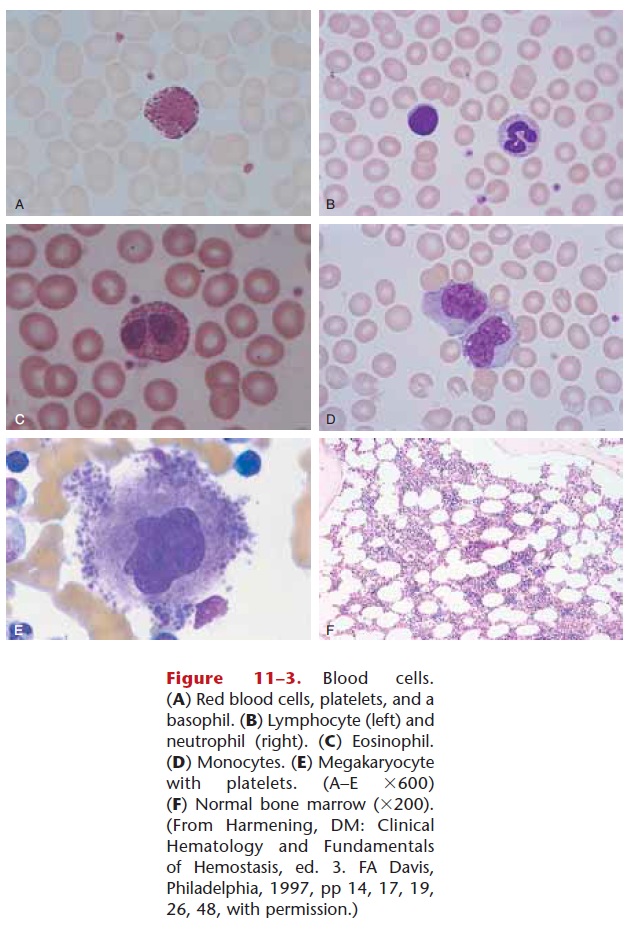
White blood cells (WBCs) are also called leukocytes. There are five kinds of WBCs; all are larger than RBCs and have nuclei when mature. The nucleus may be in one piece or appear as several lobes or segments. Special staining for microscopic examination gives each kind of WBC a distinctive appearance (see Figs. 11–2 and 11–3).
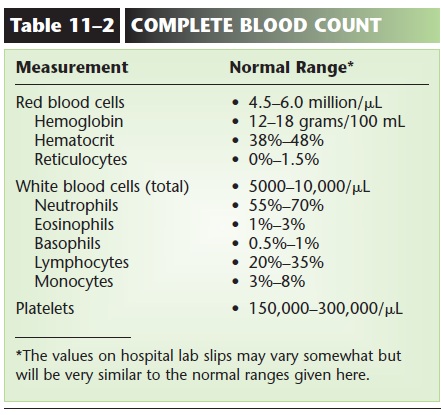
A normal WBC count (part of a CBC) is 5,000 to 10,000 per mL. Notice that this number is quite small compared to a normal RBC count. Many of our WBCs are not circulating within blood vessels but are carrying out their functions in tissue fluid or in lym-phatic tissue.
Classification
The five kinds of white blood cells, all produced in the red bone marrow (and some lymphocytes in lymphatic tissue), may be classified in two groups: granular and agranular. The granular leukocytes are the neu-trophils, eosinophils, and basophils, which usually have nuclei in two or more lobes or segments, and have distinctly colored granules when stained. Neutrophils have light blue granules, eosinophils have red granules, and basophils have dark blue granules. The agranular leukocytes are lymphocytes andmonocytes, which have nuclei in one piece. Monocytes are usually quite a bit larger than lympho-cytes. A differential WBC count(part of a CBC) is the percentage of each kind of leukocyte. Normal ranges are listed in Table 11–2, along with other nor-mal values of a CBC.
Functions
White blood cells all contribute to the same general function, which is to protect the body from infectious disease and to provide immunity to certain diseases. Each kind of leukocyte makes a contribution to this very important aspect of homeostasis.
Neutrophils and monocytes are capable of the phagocytosis of pathogens. Neutrophils are the more abundant phagocytes, but the monocytes are the more efficient phagocytes, because they differentiate into macrophages, which also phagocytize dead or dam-aged tissue at the site of any injury, helping to make tissue repair possible. During an infection, neutrophils are produced more rapidly, and the immature forms, called band cells (see Fig. 11–2), may appear in greater numbers in peripheral circulation (band cells are usually less than 10% of the total neutrophils). The term “band” refers to the nucleus that has not yet become segmented, and may look somewhat like a dumbbell.
Eosinophils are believed to detoxify foreign proteins and will phagocytize anything labeled with antibodies. This is especially important in allergic reactions and parasitic infections such as trichinosis (a worm parasite). Basophils contain granules of heparin and histamine. Heparin is an anticoagulant that helps prevent abnormal clotting within blood vessels. Histamine, you may recall, is released as part of the inflammation process, and it makes capillaries more permeable, allowing tissue fluid, proteins, and white blood cells to accumulate in the damaged area.
There are two major kinds of lymphocytes, T cells and B cells, and a less numerous third kind called nat-ural killer cells. For now we will say that T cells (or T lymphocytes) help recognize foreign antigens and may directly destroy some foreign antigens. B cells (or B lymphocytes) become plasma cells that produce anti-bodies to foreign antigens. Both T cells and B cells provide memory for immunity. Natural killer cells (NK cells) destroy foreign cells by chemically ruptur-ing their membranes. These functions of lymphocytes are discussed in the context of the mechanisms of immunity.
As mentioned earlier, leukocytes function in tissue fluid as well as in the blood. Many WBCs are capable of self-locomotion (ameboid movement) and are able to squeeze between the cells of capillary walls and out into tissue spaces. Macrophages provide a good exam-ple of the dual locations of leukocytes. Some macrophages are “fixed,” that is, stationary in organs such as the liver, spleen, and red bone marrow (part of the tissue macrophage or RE system—the same macrophages that phagocytize old RBCs) and in the lymph nodes. They phagocytize pathogens that circu-late in blood or lymph through these organs. Other “wandering” macrophages move about in tissue fluid, especially in the areolar connective tissue of mucous membranes and below the skin. Pathogens that gain entry into the body through natural openings or through breaks in the skin are usually destroyed by the macrophages and other leukocytes in connective tissue before they can cause serious disease. The alveoli of the lungs, for example, have macrophages that very efficiently destroy pathogens that enter with inhaled air.
A high WBC count, called leukocytosis, is often an indication of infection. Leukopenia is a low WBC count, which may be present in the early stages of dis-eases such as tuberculosis. Exposure to radiation or to chemicals such as benzene may destroy WBCs and lower the total count. Such a person is then very sus-ceptible to infection. Leukemia, or malignancy of leukocyte-forming tissues.
The white blood cell types (analogous to RBC types such as the ABO group) are called human leukocyte antigens (HLA), WhiteBlood Cell Types: HLA.
Related Topics