Chapter: Medical Surgical Nursing: Fluid and Electrolytes: Balance and Distribution
Sodium Deficit (Hyponatremia)
SODIUM
DEFICIT (HYPONATREMIA)
Hyponatremia refers to a
serum sodium level that is below nor-mal (less than 135 mEq/L [135 mmol/L]).
Plasma sodium con-centration represents the ratio of total body sodium to total
body water. A decrease in this ratio can occur from a low quantity of total
body sodium with a lesser reduction in total body water, normal total body
sodium content with excess total body water, and an excess of total body sodium
with an even greater excess of total body water. However, a hyponatremic state
can be super-imposed on an existing FVD or FVE.
Sodium may be lost by
way of vomiting, diarrhea, fistulas, or sweating, or it may be associated with
the use of diuretics, parti-cularly in combination with a low-salt diet. A
deficiency of aldo-sterone, as occurs in adrenal insufficiency, also predisposes
the patient to sodium deficiency.
Dilutional Hyponatremia
In water intoxication (dilutional hyponatremia), the patient’s serum
sodium level is diluted by an increase in the ratio of water to sodium. This
causes water to move into the cell, so that the pa-tient develops an ECF volume
excess. Predisposing conditions for this type of hyponatremia include syndrome
of inappropriate antidiuretic hormone (SIADH), hyperglycemia, and increased
water intake through the administration of electrolyte-poor parenteral fluids, the use
of tap-water enemas, or the irrigation of naso-gastric tubes with water instead
of normal saline solution.
Water may be gained abnormally by the excessive parenteral
administration of dextrose and water solutions, particularly dur-ing periods of
stress. It may also be gained by compulsive water drinking (psychogenic
polydipsia).
SIADH
The basic physiologic
disturbances in SIADH are excessive ADH activity, with water retention and
dilutional hyponatremia, and inappropriate urinary excretion of sodium in the
presence of hyponatremia. SIADH can be the result of either sustained
se-cretion of ADH by the hypothalamus or production of an ADH-like substance
from a tumor (aberrant ADH production).
Conditions associated
with SIADH include oat-cell lung tu-mors, head injuries, endocrine and
pulmonary disorders, physio-logic or psychological stress, and the use of
medications such as oxytocin, cyclophosphamide, vincristine, thioridazine, and
ami-triptyline.
Clinical Manifestations
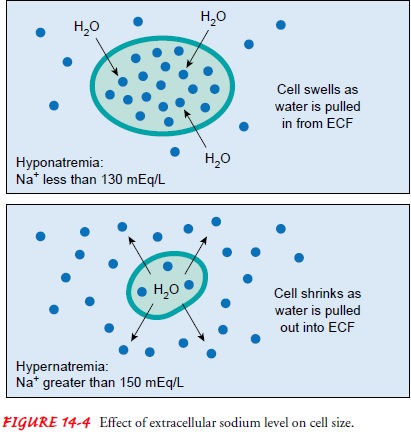
Clinical manifestations of hyponatremia depend on the cause, mag-nitude,
and speed with which the deficit occurs. Poor skin turgor, dry mucosa,
decreased saliva production, orthostatic fall in bloodpressure, nausea, and
abdominal cramping occur. Neurologic changes, including altered mental status,
are probably related to the cellular swelling and cerebral edema associated
with hyponatremia. As the extracellular sodium level decreases, the cellular
fluid be-comes relatively more concentrated and pulls water into the cells (Fig.
14-4). In general, patients with an acute decrease in serum sodium levels have
more severe symptoms and higher mortality rates than do those with more slowly
developing hyponatremia.
Features of hyponatremia associated with sodium loss and water gain
include anorexia, muscle cramps, and a feeling of ex-haustion. When the serum
sodium level drops below 115 mEq/L (115 mmol/L), signs of increasing
intracranial pressure, such as lethargy, confusion, muscle twitching, focal
weakness, hemipare-sis, papilledema, and seizures, may occur.
Assessment and Diagnostic Findings
Regardless of the cause of hyponatremia, the serum sodium level is less
than 135 mEq/L; in SIADH it may be quite low, such as 100 mEq/L (100 mmol/L) or
less. Serum osmolality is also de-creased, except in azotemia or ingestion of
toxins. When hypo-natremia is due primarily to sodium loss, the urinary sodium
content is less than 20 mEq/L (20 mmol/L), suggesting increased proximal
reabsorption of sodium secondary to ECF volume de-pletion; the specific gravity
is low, such as 1.002 to 1.004. When hyponatremia is due to SIADH, however, the
urinary sodium content is greater than 20 mEq/L and the urine specific gravity
is usually over 1.012. Although the patient with SIADH retains water abnormally
and thus gains body weight, there is no pe-ripheral edema; instead, fluid
accumulates inside the cells. This phenomenon is sometimes manifested as
“fingerprinting” when the finger is pressed over a bony prominence, such as the
sternum.
Medical Management
The key to treating hyponatremia is assessment; this includes the speed with which hyponatremia occurred rather than relying only on the patient’s actual serum sodium value (Fall, 2000).
SODIUM REPLACEMENT
The obvious treatment for hyponatremia is careful administration of
sodium by mouth, nasogastric tube, or the parenteral route. For patients who
can eat and drink, sodium is easily replaced, be-cause sodium is consumed
abundantly in a normal diet. For those who cannot consume sodium, lactated
Ringer’s solution or iso-tonic saline (0.9% sodium chloride) solution may be
prescribed. Serum sodium must not be increased by greater than 12 mEq/L in 24
hours, to avoid neurologic damage due to osmotic de-myelination. This condition
may occur when the serum sodium concentration is overcorrected (above 140
mEq/L) too rapidly or in the presence of hypoxia or anoxia (Pirzanda &
Imran, 2001). It may produce lesions in the pons that cause paraparesis,
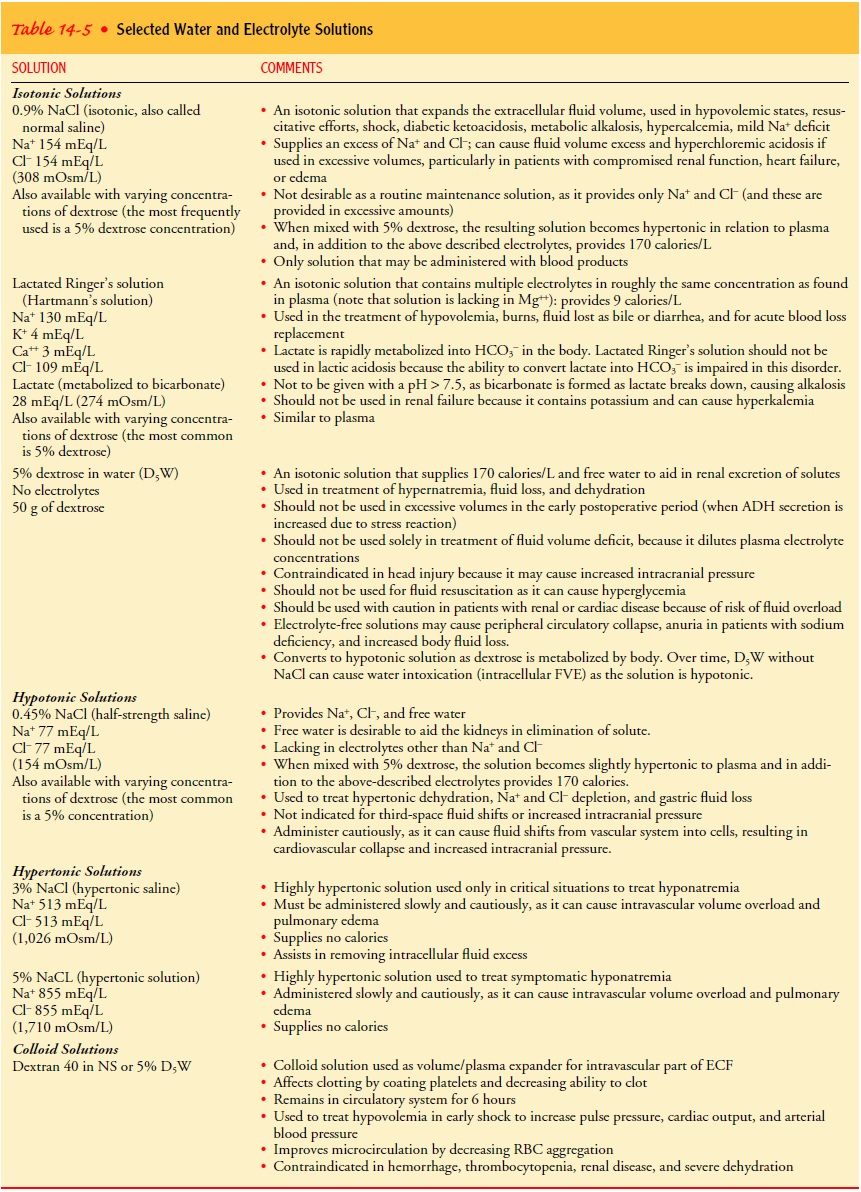
dysarthria, dysphagia, and coma. Table 14-5 describes the components of
selected water and electrolyte solutions. The usual daily sodium requirement in
adults is approximately 100 mEq, provided there are no abnormal losses.
In SIADH, the administration of hypertonic saline solution alone cannot
change the plasma sodium concentration. Excess sodium would be excreted rapidly
in a highly concentrated urine. With the addition of the diuretic furosemide
(Lasix), urine is not concentrated and isotonic urine is excreted to effect a
change in water balance. In patients with SIADH, in whom water restric-tion is
difficult, lithium or demeclocycline can antagonize the os-motic effect of ADH
on the medullary collecting tubule.
WATER RESTRICTION
In a patient with normal or excess fluid volume, hyponatremia is treated
by restricting fluid to a total of 800 mL in 24 hours. This is far safer than
sodium administration and is usually effective. When neurologic symptoms are
present, however, it may be nec-essary to administer small volumes of a
hypertonic sodium solu-tion, such as 3% or 5% sodium chloride. Incorrect use of
these fluids is extremely dangerous because 1 L of 3% sodium chloride solution
contains 513 mEq of sodium, and 1 L of 5% sodium chloride solution contains 855
mEq of sodium. If edema exists alone, sodium is restricted; if edema and
hyponatremia occur together, both sodium and water are restricted.
Nursing Management
The nurse needs to
identify patients at risk for hyponatremia so that they can be monitored. Early
detection and treatment of this disorder are necessary to prevent serious
consequences. For patients at risk, the nurse monitors fluid intake and output
as well as daily body weights. Abnormal losses of sodium or gains of water are
noted. GI manifestations, such as anorexia, nausea, vomiting, and abdominal
cramping, are also noted. The nurse must be particularly alert for central
nervous system changes, such as lethargy, confusion, muscle twitching, and
seizures. In general, more severe neurologic signs are
associated with very low sodium levels that have fallen rapidly because of
fluid over-loading. Serum sodium levels are monitored very closely in pa-tients
at risk for hyponatremia; when indicated, urinary sodium levels and specific
gravity are also monitored.
Hyponatremia is a
frequently overlooked cause of confusion in elderly patients. The elderly are
at increased risk for hypona-tremia because of changes in renal function and
subsequent de-creased ability to excrete excessive water loads. Administration
of medications causing sodium loss or water retention is a pre-disposing
factor.
DETECTING AND CONTROLLING HYPONATREMIA
For patients
experiencing abnormal losses of sodium who can consume a general diet, the
nurse encourages foods and fluids with a high sodium content. For example, broth
made with one beef cube contains approximately 900 mg of sodium; 8 oz of tomato
juice contains approximately 700 mg of sodium. The nurse also needs to be
familiar with the sodium content of par-enteral fluids (see Table 14-5).
For patients taking
lithium, the nurse observes for lithium tox-icity, particularly when sodium is
lost by an abnormal route. In such instances, supplemental salt and fluid are
administered. Be-cause diuretics promote sodium loss, patients taking lithium
are instructed not to use diuretics without close medical supervision. For all
patients on lithium therapy, adequate salt intake should be ensured.
Excess water supplements are avoided in patients receiving isotonic or
hypotonic enteral feedings, particularly if abnormal sodium loss occurs or
water is being abnormally retained (as in SIADH). Actual fluid needs are
determined by evaluating fluid in-take and output, urine specific gravity, and
serum sodium levels.
RETURNING SODIUM LEVEL TO NORMAL
When the primary problem is water retention, it is safer to restrict
fluid intake than to administer sodium. Administering sodium to a patient with
normovolemia or hypervolemia predisposes the pa-tient to fluid volume overload.
As stated previously, the nurse must monitor patients with cardiovascular
disease very closely.
In severe hyponatremia,
the aim of therapy is to elevate the serum sodium level only enough to
alleviate neurologic signs and symptoms. It is generally recommended that the
serum sodium concentration be raised no higher than 125 mEq/L (125 mmol/L) with
a hypertonic saline solution.
Related Topics