Chapter: Medical Surgical Nursing: Management of Patients With Chest and Lower Respiratory Tract Disorders
Lung Cancer (Bronchogenic Carcinoma)
Chest Tumors
Tumors
of the lung may be benign or malignant. A malignant chest tumor can be primary,
arising within the lung, chest wall, or mediastinum, or it can be a metastasis
from a primary tumor site elsewhere in the body. Metastatic lung tumors occur
frequently because the bloodstream transports cancer cells from pri-mary
cancers elsewhere in the body to the lungs.
LUNG CANCER (BRONCHOGENIC CARCINOMA)
Lung
cancer is the number-one cancer killer among men and women in the United
States, accounting for 31% of cancer deaths in men and 25% in women (American
Cancer Society, 2002; Greenlee et al., 2001). For men, the incidence of lung
cancer has remained relatively constant, but in women it continues to rise.
Lung cancer affects primarily those in the sixth or seventh decade of life;
less than 5% of patients are under the age of 40. In ap-proximately 70% of lung
cancer patients, the disease has spread to regional lymphatics and other sites
by the time of diagnosis. As a result, the long-term survival rate for lung
cancer patients is low. Evidence indicates that carcinoma tends to arise at
sites of previ-ous scarring (TB, fibrosis) in the lung. More than 85% of lung
cancers are caused by the inhalation of carcinogenic chemicals, most commonly
cigarette smoke (Schottenfeld, 2000).
Pathophysiology
Lung
cancers arise from a single transformed epithelial cell in the tracheobronchial
airways. A carcinogen (cigarette smoke, radon gas, other occupational and
environmental agents) binds to a cell’s DNA and damages it. This damage results
in cellular changes, ab-normal cell growth, and eventually a malignant cell. As
the dam-aged DNA is passed on to daughter cells, the DNA undergoes further
changes and becomes unstable. With the accumulation of genetic changes, the
pulmonary epithelium undergoes malig-nant transformation from normal epithelium
to eventual inva-sive carcinoma.
Squamous
cell carcinoma is more centrally located and arises more commonly in the
segmental and subsegmental bronchi in response to repetitive carcinogenic
exposures. Adenocarcinoma is the most prevalent carcinoma of the lung for both
men and women; it presents more peripherally as peripheral masses or nod-ules
and often metastasizes. Large cell carcinoma (also called un-differentiated
carcinoma) is a fast-growing tumor that tends to arise peripherally.
Bronchioalveolar cell cancer arises from the ter-minal bronchus and alveoli and
is usually slower growing as compared to other bronchogenic carcinomas. Lastly,
small cell carcinomas arise primarily as a proximal lesion or lesions but may
arise in any part of the tracheobronchial tree.
Classification and Staging
Non-small
cell carcinoma represents 70% to 75% of tumors; small cell carcinoma represents
15% to 20% of tumors. For non-small cell carcinoma, the cell types include squamous
cell carcinoma (30%), large cell carcinoma (10% to 16%), and adenocarcinoma
(31% to 34%), including bronchioalveolar carcinoma (3% to 4%). Most small cell
carcinomas arise in the major bronchi and spread by infiltration along the
bronchial wall. Small cell cancers account for 20% to 25% of all bronchogenic
cancers (Matthay, Tanoue & Carter, 2000).
In
addition to cell type, lung cancers also are staged. The stage of the tumor
refers to the size of the tumor, its location, whether lymph nodes are involved,
and whether the cancer has spread (American Joint Committee on Cancer, 2002).
Non-small cell lung cancer is staged as I to IV. Stage I is the earliest stage
with the highest cure rates, while stage IV designates metastatic spread.
Small
cell lung cancers are classified as limited or extensive.
Risk Factors
Various
factors have been associated with the development of lung cancer, including
tobacco smoke, second-hand (passive) smoke, environmental and occupational
exposures, gender, ge-netics, and dietary deficits. Other factors that have
been associ-ated with lung cancer include genetic predisposition and other
underlying respiratory diseases, such as COPD and TB.
TOBACCO SMOKE
Tobacco
use is responsible for more than one of every six deaths in the United States
from pulmonary and cardiovascular dis-eases. Smoking is the most important
single preventable cause of death and disease in this country. More than 85% of
lung cancers are attributable to inhalation of carcinogenic chemicals, such as
cigarette smoke (American Cancer Society, 2002). Lung cancer is 10 times more
common in cigarette smokers than non-smokers. Risk is determined by the
pack-year history (number of packs of cigarettes used each day, multiplied by
the number of years smoked), the age of initiation of smoking, the depth of
inhalation, and the tar and nicotine levels in the cigarettes smoked. The
younger a person is when he or she starts smok-ing, the greater the risk of
developing lung cancer. The risk of lung cancer decreases as the duration of
smoking cessation increases.
SECOND-HAND SMOKE
Passive
smoking has been identified as a possible cause of lung cancer in nonsmokers.
In other words, people who are involun-tarily exposed to tobacco smoke in a
closed environment (home, car, building) are at increased risk for developing
lung cancer as compared to unexposed nonsmokers. An average lifetime passive
smoke exposure to a smoking spouse or partner increases a non-smoker’s risk of
lung cancer by about 35% compared to the risk of 100% for a lifetime of active
smoking (Matthay, Tanoue & Carter, 2000).
ENVIRONMENTAL AND OCCUPATIONAL EXPOSURE
Various
carcinogens have been identified in the atmosphere, in-cluding motor vehicle
emissions and pollutants from refineries and manufacturing plants. Evidence
suggests that the incidence of lung cancer is greater in urban areas as a
result of the buildup of pollutants and motor vehicle emissions.
Radon
is a colorless, odorless gas found in soil and rocks. For many years it has
been associated with uranium mines, but it is now known to seep into homes
through ground rock. High levels of radon have been associated with the
development of lung can-cer, especially when combined with cigarette smoking.
Home-owners are advised to have radon levels checked in their houses and to
arrange for special venting if the levels are high.
Chronic
exposure to industrial carcinogens, such as arsenic, asbestos, mustard gas,
chromates, coke oven fumes, nickel, oil, and radiation, has been associated
with the development of lung cancer. Laws have been passed to control exposure
to such ele-ments in the workplace.
GENETICS
Some
familial predisposition to lung cancer seems apparent, be-cause the incidence
of lung cancer in close relatives of patients with lung cancer appears to be
two to three times that of the gen-eral population regardless of smoking
status.
DIETARY FACTORS
Prior
research has demonstrated that smokers who eat a diet low in fruits and
vegetables have an increased risk of developing lung cancer (Bast, Kufe,
Pollock et al., 2000). The actual active agents in a diet rich in fruits and
vegetables have yet to be determined. It has been hypothesized that
carotenoids, particularly carotene or vitamin A, may be important. Several
ongoing trials may help to determine if carotene supplementation has anticancer
proper-ties. Other nutrients, including vitamin E, selenium, vitamin C, fat,
and retinoids, are also being evaluated regarding their pro-tective role
against lung cancer (Bast, Kufe, Pollock et al., 2000).
Clinical Manifestations
Often,
lung cancer develops insidiously and is asymptomatic until late in its course.
The signs and symptoms depend on the location and size of the tumor, the degree
of obstruction, and the existence of metastases to regional or distant sites.
The
most frequent symptom of lung cancer is cough or change in a chronic cough.
People frequently ignore this symptom and attribute it to smoking or a
respiratory infection. The cough starts as a dry, persistent cough, without
sputum production. When obstruction of airways occurs, the cough may become
productive due to infection.
Wheezing
is noted (occurs when a bronchus becomes partially obstructed by the tumor) in
about 20% of patients with lung can-cer. Patients also may report dyspnea. Hemoptysis
or blood-tinged sputum may be expectorated. In some patients, a recurring fever
occurs as an early symptom in response to a persistent in-fection in an area of
pneumonitis distal to the tumor. In fact, can-cer of the lung should be
suspected in people with repeated unresolved upper respiratory tract
infections. Chest or shoulder pain may indicate chest wall or pleural
involvement by a tumor. Pain also is a late manifestation and may be related to
metastasis to the bone.
If
the tumor spreads to adjacent structures and regional lymph nodes, the patient
may present with chest pain and tightness, hoarseness (involving the recurrent
laryngeal nerve), dysphagia, head and neck edema, and symptoms of pleural or
pericardial ef-fusion. The most common sites of metastases are lymph nodes,
bone, brain, contralateral lung, adrenal glands, and liver. Non-specific
symptoms of weakness, anorexia, and weight loss also may be diagnostic.
Assessment and Diagnostic Findings
If
pulmonary symptoms occur in a heavy smoker, cancer of the lung is suspected. A
chest x-ray is performed to search for pul-monary density, a solitary
peripheral nodule (coin lesion), atelec-tasis, and infection. CT scans of the
chest are used to identify small nodules not visualized on the chest x-ray and
also to exam-ine serially areas of the thoracic cage not clearly visible on the
chest x-ray.
Sputum
cytology is rarely used to make a diagnosis of lung cancer; however, fiberoptic
bronchoscopy is more commonly used and provides a detailed study of the
tracheobronchial tree and allows for brushings, washings, and biopsies of
suspicious areas. For peripheral lesions not amenable to bronchoscopic biopsy,
a transthoracic fine-needle aspiration
may be performed under CT or fluoroscopic guidance to aspirate cells from a
suspi-cious area. In some circumstances, an endoscopy with esophageal
ultrasound (EUS) may be used to obtain a transesophageal biopsy of enlarged
subcarinal lymph nodes that are not easily accessible by other means.
A
variety of scans may be used to assess for metastasis of the cancer. These may
include bone scans, abdominal scans, positron emission tomography (PET) scans,
or liver ultrasound or scans. CT of the brain, magnetic resonance imaging
(MRI), and other neuro-logic diagnostic procedures are used to detect central
nervous sys-tem metastases. Mediastinoscopy or mediastinotomy may be used to
obtain biopsy samples from lymph nodes in the mediastinum.
If
surgery is a potential treatment, the patient is evaluated to determine whether
the tumor is resectable and whether the physiologic impairment resulting from
such surgery can be tol-erated. Pulmonary function tests, arterial blood gas
analysis, ventilation–perfusion scans, and exercise testing may all be used as
part of the preoperative assessment (Knippel, 2001).
Medical Management
The
objective of management is to provide a cure, if possible. Treatment depends on
the cell type, the stage of the disease, and the physiologic status
(particularly cardiac and pulmonary status) of the patient. In general,
treatment may involve surgery, radia-tion therapy, or chemotherapy—or a
combination of these. Newer and more specific therapies to modulate the immune
system (gene therapy, therapy with defined tumor antigens) are under study and
show promise in treating lung cancer.
SURGICAL MANAGEMENT
Surgical
resection is the preferred method of treating patients with localized non-small
cell tumors, no evidence of metastatic spread, and adequate cardiopulmonary
function. If the patient’s cardiovascular status, pulmonary function, and
functional status are satisfactory, surgery is generally well tolerated.
Coronary artery disease, pulmonary insufficiency, and other comorbidities,
how-ever, may contraindicate surgical intervention. The cure rate of surgical
resection depends on the type and stage of the cancer. Surgery is primarily
used for non-small cell carcinomas because small cell cancer of the lung grows
rapidly and metastasizes early and extensively. Unfortunately, in many patients
with broncho-genic cancer, the lesion is inoperable at the time of diagnosis.
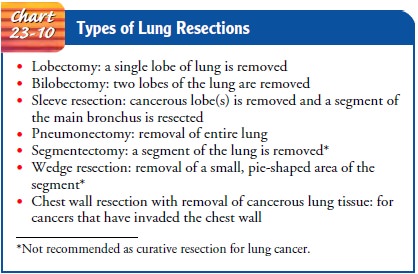
Several
different types of lung resections may be performed (Chart 23-10). The most
common surgical procedure for a small, apparently curable tumor of the lung is
lobectomy (removal of a lobe of the lung). In some cases, an entire lung may be
removed (pneumonectomy).
RADIATION THERAPY
Radiation therapy may cure a small percentage of patients. It is useful in controlling neoplasms that cannot be surgically resected but are responsive to radiation. Radiation also may be used to re-duce the size of a tumor, to make an inoperable tumor operable, or to relieve the pressure of the tumor on vital structures. It can control symptoms of spinal cord metastasis and superior vena caval compression. Also, prophylactic brain irradiation is used in certain patients to treat microscopic metastases to the brain. Ra-diation may help relieve cough, chest pain, dyspnea, hemoptysis, and bone and liver pain. Relief of symptoms may last from a few weeks to many months and is important in improving the qual-ity of the remaining period of life.
Radiation
therapy usually is toxic to normal tissue within the radiation field, and this
may lead to complications such as esophagitis, pneumonitis, and radiation lung
fibrosis. These may impair ventilatory and diffusion capacity and significantly
reduce pulmonary reserve. The patient’s nutritional status, psychologi-cal
outlook, fatigue level, and signs of anemia and infection are monitored
throughout the treatment.
CHEMOTHERAPY
Chemotherapy
is used to alter tumor growth patterns, to treat pa-tients with distant
metastases or small cell cancer of the lung, and as an adjunct to surgery or
radiation therapy. Combinations of two or more medications may be more
beneficial than single-dose regimens. A large number of medications are active
against lung cancer. A variety of chemotherapeutic agents are used, including
alkylating agents (ifosfamide), platinum analogues (cisplatin and carboplatin),
taxanes (paclitaxel, docetaxel), vinca alkaloids (vinblastine and vindesine),
doxorubicin, gemcitabine, vinorel-bine, irinotecan (CPT-11), and etoposide
(VP-16). The choice of agent depends on the growth of the tumor cell and the
specific phase of the cell cycle that the medication affects. Numerous
com-binations of chemotherapy are undergoing investigation to iden-tify the
optimal regimen to treat differing types of lung cancer.
Chemotherapy
may provide relief, especially of pain, but it does not usually cure the
disease, nor does it often prolong life to any great degree. Chemotherapy is
also accompanied by side effects. It is valuable in reducing pressure symptoms
of lung cancer and in treating brain, spinal cord, and pericardial metastasis.
PALLIATIVE THERAPY
Palliative
therapy may include radiation therapy to shrink the tumor to provide pain
relief, a variety of bronchoscopic inter-ventions to open a narrowed bronchus
or airway, and pain man-agement and other comfort measures. Evaluation and referral
for hospice care are important in planning for comfortable and dig-nified
end-of-life care for the patient and family.
Treatment-Related Complications
A
variety of complications may occur as a result of lung cancer treatments.
Radiation therapy may result in diminished cardio-pulmonary function and other
complications, such as pulmonary fibrosis, pericarditis, myelitis, and cor
pulmonale. Chemotherapy, particularly in combination with radiation therapy,
can cause pneumonitis. Pulmonary toxicity is a potential side effect of
chemotherapy. Surgical resection may result in respiratory fail-ure,
particularly when the cardiopulmonary system is compro-mised before surgery.
Surgical complications and prolonged mechanical ventilation are potential
outcomes.
Nursing Management
Nursing
care of the patient with lung cancer is similar to that of other patients with
cancer and addresses the phys-iologic
and psychological needs of the patient. The physiologic problems are primarily
due to the respiratory manifestations of the disease. Nursing care includes
strategies to ensure relief of pain and discomfort and to prevent
complications.
MANAGING SYMPTOMS
The
nurse instructs the patient and family about the potential side effects of the
specific treatment and strategies to manage them. Strategies for managing such
symptoms as dyspnea, fa-tigue, nausea and vomiting, and anorexia will assist
the patient and family to cope with the therapeutic measures.
RELIEVING BREATHING PROBLEMS
Airway
clearance techniques are key to maintaining airway patency through the removal
of excess secretions. This may be accomplished through deep-breathing
exercises, chest physiotherapy, directed cough, suctioning, and in some
instances bronchoscopy. Bron-chodilator medications may be prescribed to
promote bronchial dilation. As the tumor enlarges or spreads, it may compress a
bronchus or involve a large area of lung tissue, resulting in an im-paired
breathing pattern and poor gas exchange. At some stage of the disease,
supplemental oxygen will probably be necessary.
Nursing
measures focus on decreasing dyspnea by encourag-ing the patient to assume
positions that promote lung expansion, breathing exercises for lung expansion
and relaxation, and edu-cating the patient on energy conservation and airway
clearance techniques (Connolly & O’Neill, 1999). Many of the techniques
used in pulmonary rehabilitation can be applied to the lung can-cer patient.
Depending on the severity of disease and the patient’s wishes, a referral to a
pulmonary rehabilitation program may be helpful in managing respiratory
symptoms.
REDUCING FATIGUE
Fatigue
is a devastating symptom that affects quality of life in the cancer patient. It
is commonly experienced by the lung cancer pa-tient and may be related to the
disease itself, the cancer treatment and complications (eg, anemia), sleep
disturbances, pain and dis-comfort, hypoxemia, poor nutrition, or the
psychological ramifi-cations of the disease (eg, anxiety, depression). The
nurse is pivotal in thoroughly assessing the patient’s level of fatigue,
identifying potentially treatable causes, and validating with the patient that
fatigue is indeed an important symptom. Educating the patient in energy
conservation techniques or referring the patient to a physical therapy, occupational
therapy, or pulmonary rehabilita-tion program may be helpful. In addition,
guided exercise has been recently identified as a potential intervention for
treating fatigue in cancer patients. This is an important area for research
because few studies have been conducted, and only in select pop-ulations of
cancer patients.
PROVIDING PSYCHOLOGICAL SUPPORT
Another
important part of the nursing care of the patient with lung cancer is
psychological support and identification of poten-tial resources for the
patient and family. Often, the nurse must help the patient and family deal with
the poor prognosis and rel-atively rapid progression of this disease. The nurse
must help the patient and family with informed decision making regarding the
possible treatment options, methods to maintain the patient’s quality of life
during the course of this disease, and end-of-life treatment options.
Related Topics