Chapter: Medicine Study Notes : Renal and Genitourinary
Acute Renal Failure - Kidney Disease
Acute Renal Failure
· =Abrupt reduction in glomerular filtration rate ® plasma urea & creatinine and (usually) ¯urine volume (oliguria < 400 ml/day, auria < 100 ml/day). If urea but only Cr then ?dehydration or catabolic state
· Assess severity using Cockcroft-Gault equation . Normal clearance >= ~ 100 ml/min
· Due to acute damage to any part of the kidney or renal tract. Usually Acute Tubular Necrosis but always consider differentials
Pre-renal Acute Renal Failure
· =¯ in glomerular perfusion in absence of structural kidney damage
· Kidney usually autoregulates – but can‟t cope with extremes
· Can‟t interpret results if patient has had recent diuretics
· If prolonged ® ischaemic damage ® loss of medullary gradient and reabsorbing capacity ® dilute urine
· Causes:
o Volume depletion: Usually GI loss, but also renal loss, burns, haemorrhage
o Cardiac failure ® ¯renal perfusion
o Systemic vasodilation: sepsis or antihypertensives
o Also:
§ Reno-vascular disease: renal artery stenosis
§ Vasoconstriction in kidneys, e.g. due to NSAIDs (® ¯vasodilating PGs), ACE inhibitors (® ¯efferent arteriolar tone® ¯intraglomerular pressure)
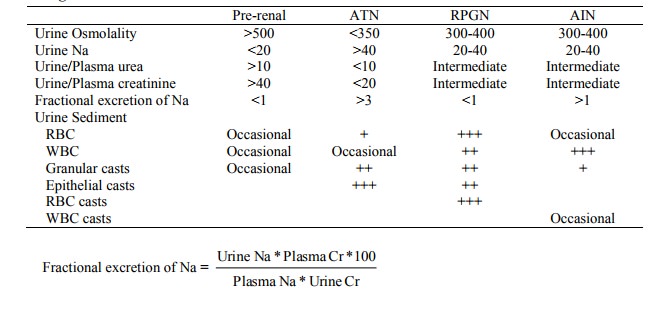
· Intense reabsorption of salt and water leads to:
o Low volume of urine, high osmolality (> plasma), but low urine Na (usually < 20 mmol/l)
o Urine to plasma ratio of creatinine and urea
o Urea is re-absorbed preferentially to creatinine at low urine flows Þ plasma urea to creatinine is increased
o Hyaline casts: aggregations of urine protein if low urine flow
· Kidneys try to compensate by:
o Vasodilating afferent arterioles (via PGs)
o Activation of renin-angiotensin ® BP and vasoconstricts efferent arterioles
· Management:
o Rapid fluid resuscitation
o Correct underlying disorder (eg inotropes)
o Monitor intravascular volume and watch for ATN
Intrinsic Acute Renal Failure
· Possible presentations:
o Oliguria (rather than auria)
o Nephritic syndrome: haematuria, hypertension, oliguria +/- oedema
o Proteinuria: excludes pre and post-renal
o Hypertension: intrinsic renal disease ® BP, pre-renal ® ¯BP
o Systemic features of disorders causing intrinsic failure (eg fever, arthralgia, skin rash, vasculitis etc)
· Due to:
o Acute Tubular Necrosis (most common cause)
o Acute Interstitial Nephritis
o RPGN: Urine chemistry midway between pre-renal acute renal failure and acute tubular necrosis - urine to plasma ratios for osmolality and creatinine, and Na between 20 – 40 mmol/L.
o Nephrotoxins
o Other tubular diseases (eg myeloma)
· Investigations:
o Urinalysis: cells, casts, protein
o US: echogenicity
o Renal biopsy
o Also blood tests to exclude specific causes: ANA, ANCA, Complement, CK, etc
Post-renal Acute Renal Failure
· Presentation:
o Complete auria: most pre-renal and intra-renal failure is oliguric. But partial obstruction may give moderate tubular dysfunction ® osmotic diuresis ® polyuria
o Normal urinalysis: no proteinuria or casts, any blood (eg from stones, cancer) will be normal not dysmorphic
o Specific diseases pre-dispose: eg diabetes and analgesic use ® papillary necrosis ® bits fall off and cause obstruction.
· Due to obstruction:
o Usually in urethra: bladder stones or tumours. Prostate usually chronic
o If at ureteric level must be bilateral to lead to severe kidney failure or obstruction on one side and a poor functioning kidney on the other
o Extrinsic obstruction due to eg retroperitoneal fibrosis following radiotherapy, etc
· ® tubular pressure ® ¯glomerula filtration
· Usually obvious from history, confirm with:
o Ultrasound of kidneys for hydronephrosis
o CT to determine the level of the blockage
o IVU only if the kidney is functioning (ie Cr < 200)
Investigations in Acute Renal Failure
· Renal biopsy is rarely needed to differentiate causes of renal failure, mainly in RPGN
Management
· Treat cause
· Resuscitate if hypovolaemia
· Monitor for K
· Treat pulmonary oedema, ?dialysis
· Monitor fluid balance carefully
· Avoid nephrotoxic drugs
Related Topics