Chapter: Obstetrics and Gynecology: Vulvar and Vaginal Disease and Neoplasia
Vulvar Intraepithelial Neoplasia
VULVAR INTRAEPITHELIAL NEOPLASIA
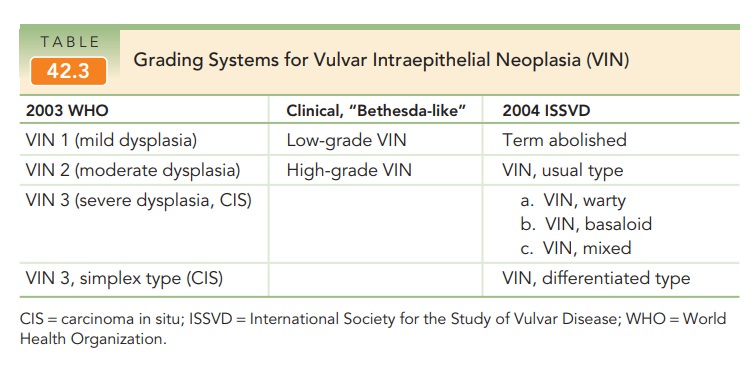
Much like the vulvar dermatoses, the classification and ter-minology of VIN is still evolving and has undergone multi-ple revisions and reclassifications over the years. There are currently three grading systems: (1) the World Health Organization (WHO) three-grade system of VIN 1, 2, and 3; (2) the clinical, Bethesda-like, two-grade system of low- and high-grade vulvar intraepithelial lesions; and the revised 2004 International Society for the Study of Vulvar Disease (ISSVD) classification, which divides VIN into two types: usual and differentiated. VIN, usual type is further divided into 3 subtypes: warty, basaloid, and mixed. These grading systems are summarized in Table 42.3.
VIN 1
VIN 1, or mild dysplasia, is a low-grade lesion that demon-strates minimal to mild squamous atypia limited to the lower epidermis. VIN 1 is either a non-neoplastic, reactive atypia or is an effect of a human papillomavirus (HPV) infection.
VIN 1 occurs most often in condylomata acumi-nata. Lesions
that are condylomatous in origin do not have the features of attenuated
maturation, pleomorphism, and atypical mitotic figures that are other forms of
VIN.
Because the features of VIN 1 are
an uncommon his-tologic finding and there is little evidence that VIN 1 is a
cancer precursor, it may be misleading to classify these lesions as true
intraepithelial neoplasia. In 2004, the ISSVD abolished the term VIN 1 from their classification system. The diagnosis of VIN 1 must be made by
biopsy, and treatment is the same as for condyloma.
VIN, Usual Type
The ISSVD combined VIN 2 and 3 into VIN, usual type. These are high-grade, HPV-related lesions distinguished only by degree of abnormality. They represent true neo-plasia with a high predilection for progression to severe intraepithelial lesions and, eventually, carcinoma, if left untreated.
Almost 60% of women with VIN 3 or
vaginal intraepithelial neoplasia (VAIN) 3 will also have cervical
intraepithelial neoplasia (CIN) lesions. Furthermore, 10% of women with CIN 3
will have either VIN or VAIN.
Smoking or secondhand smoke is a
common social-history finding in patients with VIN. Presenting complaintsinclude vulvar pruritus, chronic irritation, and a
development of raised mass lesions. Normally, the lesions are localized,
fairlywell-isolated, and raised above the normal epithelial sur-face to include
a slightly rough texture. They are usually found along the posterior, hairless
area of vulva and in the perineal body, but can occur anywhere on the vulva.
The color changes in these lesions range from white, hyperplas-tic areas to reddened
or dusky, patch-like involvement, depending on whether associated
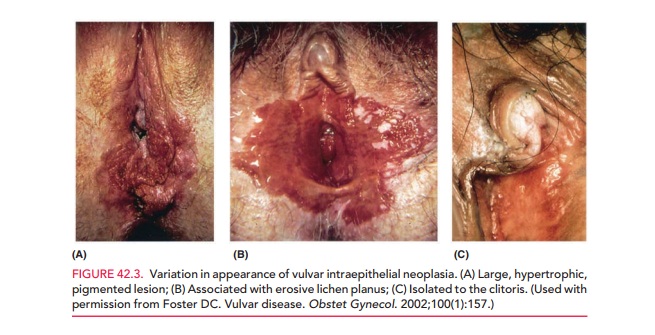
hyperkeratosis is present. Figure 42.3 illustrates the variation in appearance
of VIN.
In patients without obvious
raised or isolated lesions, careful inspection of the vulva is warranted, using
a colpo-scope. Applying a 3%- to 5%-solution of acetic acid to the vulva for 2
to 5 minutes often accentuates the white lesions and may also help in revealing
abnormal vascular patterns. These areas
must be selectively biopsied in multiple sites to thor-oughly investigate the
type of VIN and reliably exclude invasive carcinoma.
VIN, usual type is subdivided
into three histologic subtypes–warty, basaloid, or mixed–depending on the
fea-tures present. They all have atypical mitotic figures and nuclear
pleomorphism, with loss of normal differentiation in the lower one third to one
half of the epithelial layer. Full-thickness loss of maturation indicates
lesions that are at least severely dysplastic, including areas that may
rep-resent true carcinoma in situ (CIS).
The goal
in treating VIN, usual type is to quickly and com-pletely remove all involved
areas of skin. These lesions can beremoved after appropriate
biopsies confirm the absence of invasive cancer. Removal options include wide
local exci-sion or laser ablation. A variety of nonsurgical treatments for
patients with VIN, usual type have been reported, including corticosteroids,
5-fluorouracil, and imidazo-quinolones (particularly imiquimod). Results to
date are inconclusive. Careful evaluation
to exclude invasive disease isof paramount importance, as VIN, usual type is
seen adjacent to 30% of SCCs of the vulva.
VIN, Differentiated Type
The less common simplex type of
VIN (CIS) in the WHO system is now called VIN,
differentiated type by the ISSVD (see Table 42.3). The lesion is either a
hyper-keratotic plaque, warty papule, or an ulcer, seen primarily in older
women. It is often associated with keratinizing SCCs or lichen sclerosus, and
is not HPV-related. It is thought that VIN, differentiated type is
underdiagnosed due to a relatively short intraepithelial phase before
pro-gression to invasive carcinoma. Clinical awareness of this entity and its
features as different from VIN, usual type would help to improve diagnosis
before cancer has super-vened. Biopsy is mandatory and the mainstay of
treat-ment is excision.
Related Topics