Chapter: Obstetrics and Gynecology: Vulvar and Vaginal Disease and Neoplasia
Vulvar Cancer
VULVAR CANCER
Vulvar carcinoma accounts for approximately 5% of
all gyne-cologic malignancies. Approximately 90% of these
carcinomasare squamous cell carcinomas.
The second most common variety is melanoma, which accounts for 2% of all vulvar
car-cinomas, followed by sarcoma. Less-common types include basal cell
carcinoma and adenocarcinoma.
The typical clinical profile of
vulvar carcinoma includes women in their postmenopausal years, most commonly
between the ages of 70 and 80. However, about 20% of these cancers are
discovered in women younger than 50 years of age. Vulvar pruritus is the most common presenting complaint. In
addition, patients may notice a red or white ulcerative or exophytic lesion
arising most commonly on the posterior two-thirds of either labium majus. An
exophytic ulcerative lesion need not be present, further underscoring the need
for thorough biopsy in patients of the age group who com-plain of vulvar
symptoms. Patients in this older age
group maybe reluctant to consult their physicians about these signs and
symp-toms, and physicians are further reluctant to investigate the symp-toms
and findings thoroughly via vulvar biopsy, which can result in a delay in
treatment.
Although a specific cause for
vulvar cancer is not known, progression has been shown from prior intraepithe-lial
lesions, including those that are associated with certain types of HPV. Smokers
have a high preponderance in this population of patients.
Natural History
Squamous cell carcinoma of the vulva generally remains localized for long periods of time and then spreads in a pre-dictable fashion to the regional lymph nodes, including those of the inguinal and femoral chain. Lesions 2 cm wide and 0.5 cm deep have an increased chance of nodal metas-tases. The overall incidence of lymph node metastasis is approximately 30%. Lesions arising in the anterior one-third of the vulva may spread to the deep pelvic nodes, bypassing regional inguinal and femoral lymphatics.
Evaluation
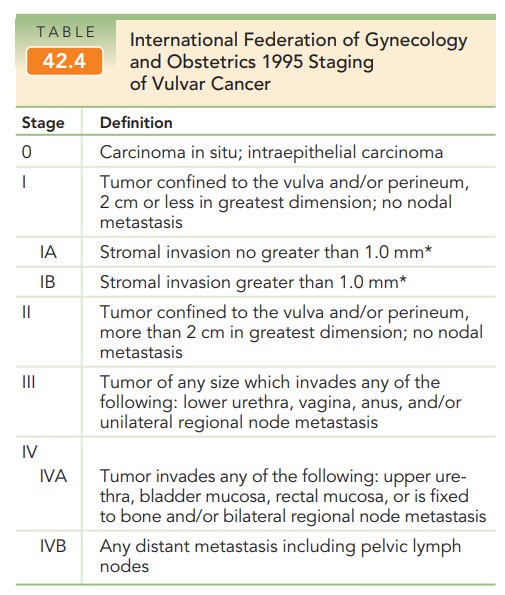
The staging classification for vulvar cancer was revised by the Federation of Gynecology and Obstetrics (FIGO) in 1995 (Table 42.4). Prior to 1988, vulvar cancers were staged clinically. However, noted discrepancies in regard to pre-dicting nodal metastasis led to a change from clinical to surgical staging. This staging convention uses the analysis of the removed vulvar tumor and microscopic assessment of the regional lymph nodes as its basis.
Treatment
Although the mainstay for the
treatment of invasive vul-var cancer is surgical,
many advances have been made to help individualize patients into treatment
categories in an effort to reduce the amount of radical surgery, while not
compromising survival. Accordingly, not all patients undergo radical vulvectomy
with bilateral nodal dissec-tions. Individualized approaches include the
following:
· Conservative
vulvar operations for unifocal lesions
· Elimination
of routine pelvic lymphadenectomy
· Avoidance
of groin dissection in unilateral lesions 1 mm deep
· Elimination
of contralateral groin dissection in unilateral lesions 1 cm from the midline
with negative ipsilateral nodes
· Separate
groin incisions for patients with indicated bilat-eral groin dissection
· Postoperative
radiation therapy to decrease groin recur-rence in patients with two or more
positive groin nodes
Concomitant use of radiation and
chemotherapy (5-fluorouracil plus cisplatin or mitomycin or cisplatin alone) is
gaining favor for treatment of vulvar cancers that require radiation therapy.
Treatment with chemotherapy in cases of recurrent vulvar cancer has only
limited value.
Prognosis
The corrected 5-year survival
rate for all vulvar carcinoma is approximately 70%. Five-year survival rates
for squa-mous cell cancer are 60% to 80% for stage I and II disease. Survival
rates for patients with stage III disease are 45%, and those with stage IV have
rates of 15%.
Other Types of Vulvar Cancer
MELANOMA
Melanoma is the most common nonsquamous
cell cancer of thevulva. Vulvar melanoma usually presents
with a raised, irri-tated, pruritic, pigmented lesion. Most commonly,
mela-notic lesions are located on the labia minora or the clitoris. Melanoma
accounts for approximately 6% of all vulvar malignancies, and when suspected,
wide local excision is necessary for diagnosis and staging. Survival approaches
100% when the lesions are confined to the intrapapillary ridges, decreasing
rapidly as involvement includes the pap-illary dermis, reticular dermis, and
finally subcutaneous tissues. In the latter instance, survival is generally 20%
because of substantial incidence of nodal involvement. Because early diagnosis
and treatment by wide excision are so crucial, it is important to recognize
that irritated, pig-mented, vulvar lesions mandate excisional biopsy for
defin-itive treatment.
CARCINOMA OF THE BARTHOLIN GLAND
Carcinoma
of the Bartholin gland is uncommon (1% to2% of all
vulvar carcinomas). Malignancies that arise from the Bartholin gland include
adenocarcinomas, squamous cell carcinomas, adenosquamous carcinomas, and
adenoid cystic and transitional-cell carcinomas. These arise mainly as a result
of changes occurring within the different histo-logic areas of the gland and
ducts leading from it. Bartholin carcinoma on average occurs in women over the
age of 50; however, any new Bartholin mass in a woman over the age of 40 should
be excised. Treatment of diagnosed Bartholin cancers is radical vulvectomy and
bilateral lymphadenec-tomy. Recurrence is disappointingly common, and a 5-year
overall survival rate of 65% is noted.
Related Topics