Chapter: Obstetrics and Gynecology: Vulvar and Vaginal Disease and Neoplasia
Lichen Simplex Chronicus - Benign Vulvar Disease
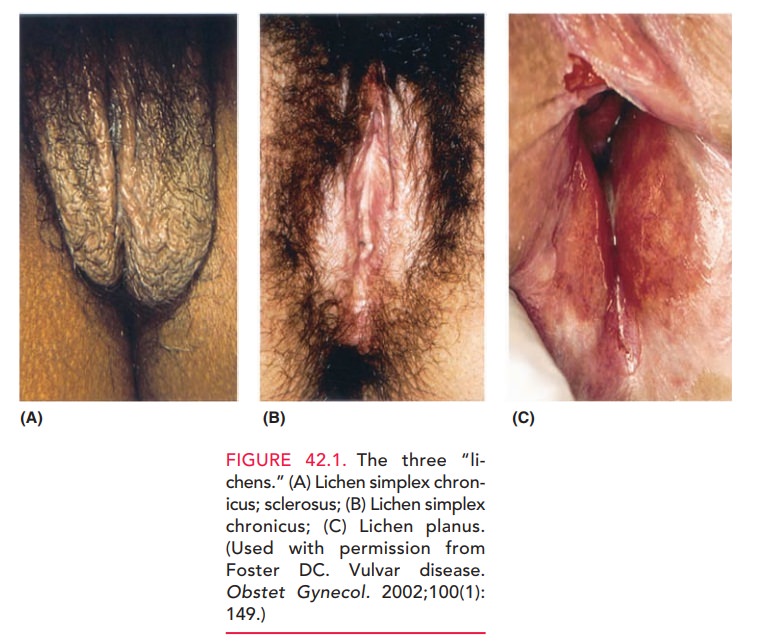
Lichen Simplex Chronicus
In contrast to many dermatologic
conditions that may be described as “rashes that itch,” lichen simplex
chronicus can be described as “an itch
that rashes.” Most patients develop this disorder secondary to an irritant
dermatitis, which progresses to lichen simplex chronicus as a result of the
effects of chronic mechanical irritation from scratch-ing and rubbing an already
irritated area. The mechanicalirritation
contributes to epidermal thickening or hyperplasia and inflammatory cell
infiltrate, which, in turn, leads to heightened sensitivity that triggers more
mechanical irritation.
Accordingly,
the history of these patients is one of progres-sive vulvar pruritus and/or
burning, which is temporarilyrelieved by scratching or
rubbing with a washcloth or some similar material. Etiologic factors for the
original pruritic symptoms often are unknown, but may include sources of skin
irritation such as laundry detergents, fab-ric softeners, scented hygienic
preparations, and the use of colored or scented toilet tissue. These potential
sources of symptoms must be investigated. Any domestic or hygienic irritants
must be removed, in combination with treatment, to break the cycle described.
On
clinical inspection, the skin of the labia majora, labia minora, and perineal
body often shows diffusely reddened areas with occasional hyperplastic or
hyperpigmented plaques of red to reddish brown (see Fig.
42.1A). One may also find occasionalareas of linear hyperplasia, which show the
effect of grossly hyperkeratotic ridges of epidermis. Biopsy of patients who
have these characteristic findings is usually not warranted.
Empiric treatment to include
antipruritic medications such as diphenhydramine hydrochloride (Benadryl) or
hydroxyzine hydrochloride (Atarax) that inhibit nighttime, unconscious
scratching, combined with a mild to moder-ate topical steroid cream applied to
the vulva, usually pro-vides relief. A steroid cream, such as hydrocortisone
(1% or 2%) or, for patients with significant areas of obvious hyperkeratosis,
triamcinolone acetonide or betamethasone valerate may be used. If significant relief is not obtained
within3 months, diagnostic vulvar biopsy is warranted.
The
prognosis for this disorder is excellent when the offend-ing irritating agents
are removed and a topical steroid prepara-tion is used appropriately. In most
patients, these measurescure the problem and eliminate future recurrences.
Related Topics