Chapter: Obstetrics and Gynecology: Vulvar and Vaginal Disease and Neoplasia
Dermatitis - Benign Vulvar Disease
Dermatitis
Vulvar
dermatitis falls into two main categories: eczema and seborrheic
dermatitis. Eczema can be further sub-divided into exogenous and endogenous
forms. Irritant and allergic contact
dermatitis are forms of exogenous eczema. They are usually reactions to
potential irritants or allergens found in soaps, laundry detergents, textiles,
and feminine hygiene products. Careful history can be helpful in identifying
the offending agent and in preventing recur-rences. Atopic dermatitis is a form of endogenous eczema that often affects
multiple sites, including the flexural sur-faces of the elbows and knees,
retroauricular area, and scalp. The lesions associated with these three forms
of dermatitis can appear similar: symmetric eczematous lesions, with underlying
erythema. Histology alone will not distinguish these three types of dermatitis.
They all exhibit a spongi-otic pattern characterized
by intercellular edema withinthe epidermis, causing widening of the space
between the cells. Therefore, these entities must often be distinguished
clinically.
Although seborrheic dermatitis is a common
problem, iso-lated vulvar seborrheic dermatitis is rare. It
involves a chronicinflammation of the sebaceous glands, but the exact cause is
unknown. The diagnosis is usually made in patients com-plaining of vulvar pruritus
who are known to have sebor-rheic dermatitis in the scalp or other hair-bearing
areas of the body. The lesion may mimic other entities such as pso-riasis or
lichen simplex chronicus. The lesions are
pale red toa yellowish pink and may be covered by an oily appearing, scaly
crust. Because this area of the body remains continuallymoist, occasional
exudative lesions include raw “weeping” patches, caused by skin maceration,
which are exacerbated by the patient’s scratching. As with psoriasis, vulvar biopsy isusually not needed when the
diagnosis is made in conjunction with known seborrheic dermatitis in other
hair-bearing areas. Thehistologic features of seborrheic dermatitis are a
combina-tion of those seen in the acanthotic and spongiotic patterns.
Treatment for vulvar dermatitis
involves removing the offending agent, if applicable, initial perineal hygiene
and the use of a 5% solution of aluminum acetate several times a day, followed
by drying. Topical corticosteroid lotions or creams containing a mixture of an
agent that penetrates well, such as betamethasone valerate, in conjunction with
crotamiton, can be used for symptom control. As with LSC, the use of
antipruritic agents as a bedtime dose in the first 10 days to 2 weeks of
treatment frequently helps break the sleep/scratch cycle and allows the lesions
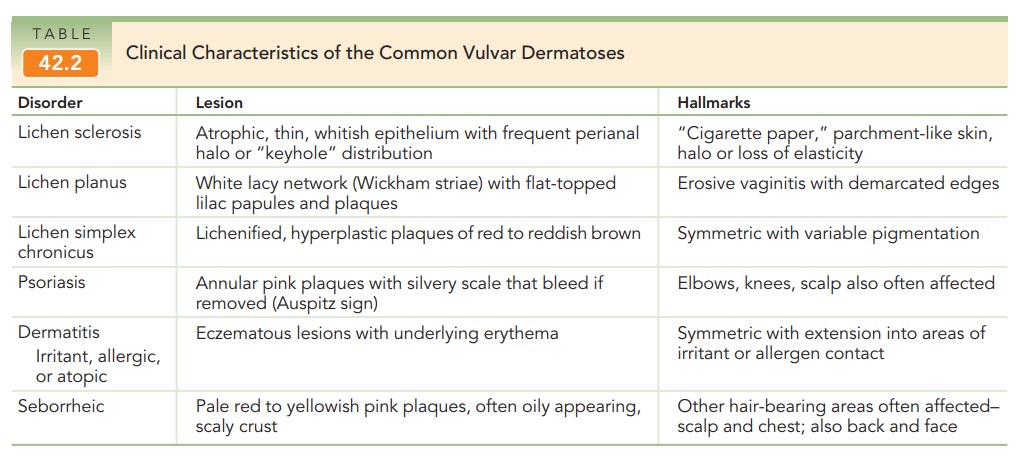
to heal. Table 42.2 summarizes the clinical characteristics of the common
vul-var dermatoses.
Related Topics