Chapter: Obstetrics and Gynecology: Vulvar and Vaginal Disease and Neoplasia
Benign Vulvar Disease
BENIGN VULVAR DISEASE
In the past, the classification
of benign, noninfectious vulvar disease used descriptive terminology based on
gross clinical morphologic appearance such as leukoplakia, kraurosis vulvae,
and hyperplastic vulvitis. Currently, these diseases are classified into three
categories: squamous cell hyperplasia, lichen sclerosus, and other dermatoses.
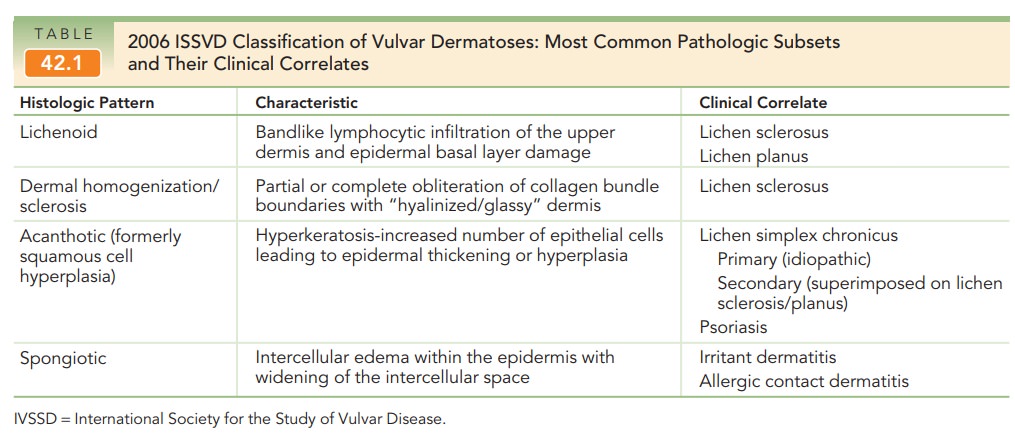
In 2006, the International Society for the Study of Vulvar Disease (ISSVD) constructed a new classification using histologic morphology based on consensus among gynecologists, dermatologists, and pathologists involved in the care of women with vulvar disease. Common ISSVD classifications are outlined in Table 42.1.
Lichen Sclerosus
Lichen
sclerosus has confused clinicians and pathologistsbecause of
inconsistent terminology and its frequent asso-ciation with other types of
vulvar pathology, including those of the acanthotic variety. As with the other
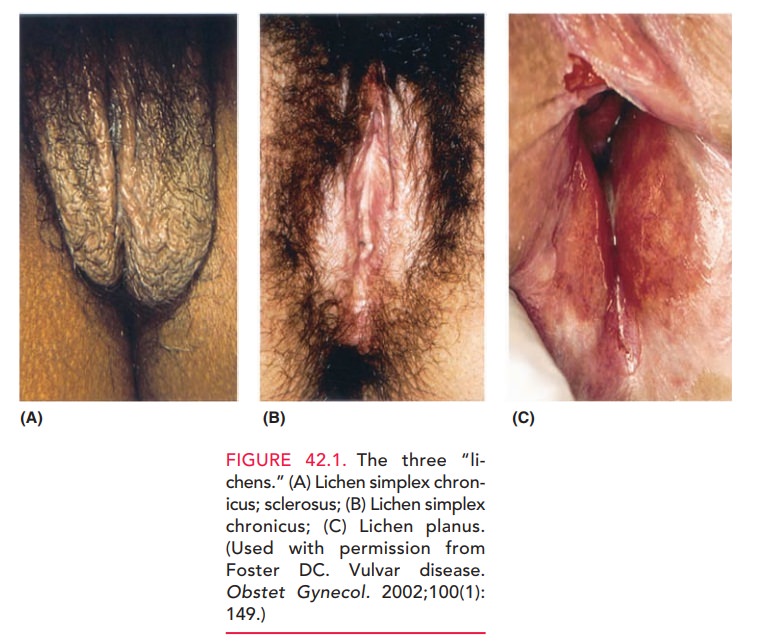
disorders, chronic vulvar pruritus occurs in most patients. Typically,the vulva is diffusely involved,
with very thin, whitish epithe-lial areas, termed “onion skin” epithelium (Fig.
42.1B). Theepithelium has been termed “cigarette paper” skin and described as
“parchment-like.” Most patients have involve-ment on both sides of the vulva,
with the most common sites being the labia majora, labia minora, the clitoral
and periclitoral epithelium, and the perineal body. The lesion may extend to
include a perianal “halo” of atrophic, whitish epithelium, forming a figure-8
configuration with the vul-var changes. In
severe cases, many normal anatomic landmarksare lost, including obliteration of
the labial and periclitoral archi-tecture as well as severe stenosis of the
vaginal introitus. Somepatients have areas of cracked skin, which are prone
to bleeding with minimal trauma. Patients with these severe anatomic changes
complain of difficulty in having normal coital function.
The
etiology of lichen sclerosus is unknown, but a familial association has been
noted, as well as disorders of the immune
However,
the response to topical steroids furtherindicates the underlying inflammatory
process and the role of prostaglandins and leukotrienes in the hallmark symptom
of pruritus. Histologic evaluation and
confirmation of lichen scle-rosis is often necessary and useful, because they
allow specific ther-apy. The histologic features of the lichenoid pattern
includea band of chronic inflammatory cells, consisting mostly of lymphocytes,
in the upper dermis with a zone of homoge-neous, pink-staining, collagenous-like
material beneath the epidermis due to cell death. The obliteration of
boundaries between collagen bundles gives the dermis a “hyalinized” or “glassy”
appearance. This dermal homogenization/ sclerosis pattern is virtually
pathognomonic.
In 27% to 35% of patients, there are associated areas of acanthosis characterized by hyperkeratosis—an increase in the number of epithelial cells (keratinocytes) with flat-tening of the rete pegs.
These areas may be mixed through-out or adjacent to the typically
lichenoid areas. In patients with this mixed pattern, both components need to
be treated to effect resolution of symptoms. Patients in whom a large
acanthotic component has been histologically confirmed should be treated
initially with well-penetrating cortico-steroid creams. With improvement of
these areas (usually 2 to 3 weeks), therapy can then be directed to the
lichenoid component.
Treatment
for lichen sclerosis includes the use of topical steroid (clobetasol)
preparations in an effort to ameliorate symp-toms. The
lesion is unlikely to resolve totally. Intermittenttreatment may be needed
indefinitely, which is in marked contrast to acanthotic lesions, which usually
totally resolve within 6 months.
Lichen
sclerosus does not significantly increase the patient’s risk of developing
cancer.
It has been estimated that this
risk is in the 4% range. However, due to the frequent coexistence with
acanthosis, the condition needs to be followed carefully and a rebiopsy
performed, because therapeutically resistant acanthosis can be a harbinger of
squamous cell carcinoma (SCC).
Lichen Simplex Chronicus
In contrast to many dermatologic
conditions that may be described as “rashes that itch,” lichen simplex
chronicus can be described as “an itch
that rashes.” Most patients develop this disorder secondary to an irritant
dermatitis, which progresses to lichen simplex chronicus as a result of the
effects of chronic mechanical irritation from scratch-ing and rubbing an already
irritated area. The mechanicalirritation
contributes to epidermal thickening or hyperplasia and inflammatory cell
infiltrate, which, in turn, leads to heightened sensitivity that triggers more
mechanical irritation.
Accordingly,
the history of these patients is one of progres-sive vulvar pruritus and/or
burning, which is temporarilyrelieved by scratching or
rubbing with a washcloth or some similar material. Etiologic factors for the
original pruritic symptoms often are unknown, but may include sources of skin
irritation such as laundry detergents, fab-ric softeners, scented hygienic
preparations, and the use of colored or scented toilet tissue. These potential
sources of symptoms must be investigated. Any domestic or hygienic irritants
must be removed, in combination with treatment, to break the cycle described.
On
clinical inspection, the skin of the labia majora, labia minora, and perineal
body often shows diffusely reddened areas with occasional hyperplastic or
hyperpigmented plaques of red to reddish brown (see Fig.
42.1A). One may also find occasionalareas of linear hyperplasia, which show the
effect of grossly hyperkeratotic ridges of epidermis. Biopsy of patients who
have these characteristic findings is usually not warranted.
Empiric treatment to include
antipruritic medications such as diphenhydramine hydrochloride (Benadryl) or
hydroxyzine hydrochloride (Atarax) that inhibit nighttime, unconscious
scratching, combined with a mild to moder-ate topical steroid cream applied to
the vulva, usually pro-vides relief. A steroid cream, such as hydrocortisone
(1% or 2%) or, for patients with significant areas of obvious hyperkeratosis,
triamcinolone acetonide or betamethasone valerate may be used. If significant relief is not obtained
within3 months, diagnostic vulvar biopsy is warranted.
The
prognosis for this disorder is excellent when the offend-ing irritating agents
are removed and a topical steroid prepara-tion is used appropriately. In most
patients, these measurescure the problem and eliminate future recurrences.
Lichen Planus
Although lichen planus is usually a desquamative lesion of the vagina,
occasional patients develop lesions on the vulva near the inner aspects of the
labia minora and vulvar vestibule. Patients may have areas of whitish, lacy
bands (Wickham striae) of keratosis near the reddish ulcerated-like lesions
characteristic of the disease (see Figure 42.1C). Typically, complaints include chronic vulvar burning and/or pruritus
and insertional (i.e., entrance) dyspareunia and a pro-fuse vaginal discharge. Because
of the patchiness of thislesion and the concern raised by atypical appearance
of the lesions, biopsy may be warranted to confirm the diagnosis in some
patients. In lichen planus, biopsy shows no atypia. Examination of the vaginal
discharge in these patients fre-quently reveals large numbers of acute
inflammatory cells without significant numbers of bacteria. Accordingly, the
diagnosis most often can be made by the typical history of vaginal/vulvar
burning and/or insertional dyspareunia, coupled with a physical examination
that shows the bright red patchy distribution; and a wet prep that shows large
numbers of white cells. Histologically the epithelium is thinned, and there is
a loss of the rete ridges with a lym-phocytic infiltrate just beneath,
associated with basal cell liquefaction necrosis.
Treatment for lichen planus is
topical steroid prepa-rations similar to those used for lichen simplex
chronicus. This may include the use of intravaginal 1% hydrocorti-sone douches.
Length of treatment for these patients is often shorter than that required to
treat lichen simplex chronicus, although lichen planus is more likely to recur.
Psoriasis
Psoriasis is an autosomal dominant
inherited disorder that caninvolve the vulvar skin as part of a generalized
dermatologic process. With approximately 2% of the
general populationsuffering from psoriasis, the physician should be alert to
its prevalence and the likelihood of vulvar manifestation, because it may
appear during menarche, pregnancy, and menopause.
The lesions are typically
slightly raised round or ovoid patches with a silver scale appearance atop an
erythema-tous base. These lesions most often measure approximately 1 × 1 to 1 × 2 cm. Though pruritus is usually
minimal, these silvery lesions will reveal punctate bleeding areas if removed
(Auspitz sign). The diagnosis is
generally known because ofpsoriasis found elsewhere on the body, obviating the
need for vul-var biopsy to confirm the diagnosis. Histologically, a
prominentacanthotic pattern is seen,
with distinct dermal papillaethat are clubbed and chronic inflammatory cells
between them.
Treatment often occurs in
conjunction with consulta-tion by a dermatologist. Like lesions elsewhere,
vulvar lesions usually respond to topical coal tar preparations, followed by
exposure to ultraviolet light as well as cortico-steroid medications, either
topically or by intralesional injection. Coal tar preparations are extremely
irritating to the vagina and labial mucous membranes and should not be used in
these areas. Because vulvar application
of some of thephotoactivated preparations can be somewhat awkward, topical
steroids are most effective, using compounds such as betametha-sone valerate
0.1%.
Dermatitis
Vulvar
dermatitis falls into two main categories: eczema and seborrheic
dermatitis. Eczema can be further sub-divided into exogenous and endogenous
forms. Irritant and allergic contact
dermatitis are forms of exogenous eczema. They are usually reactions to
potential irritants or allergens found in soaps, laundry detergents, textiles,
and feminine hygiene products. Careful history can be helpful in identifying
the offending agent and in preventing recur-rences. Atopic dermatitis is a form of endogenous eczema that often affects
multiple sites, including the flexural sur-faces of the elbows and knees,
retroauricular area, and scalp. The lesions associated with these three forms
of dermatitis can appear similar: symmetric eczematous lesions, with underlying
erythema. Histology alone will not distinguish these three types of dermatitis.
They all exhibit a spongi-otic pattern characterized
by intercellular edema withinthe epidermis, causing widening of the space
between the cells. Therefore, these entities must often be distinguished
clinically.
Although seborrheic dermatitis is a common
problem, iso-lated vulvar seborrheic dermatitis is rare. It
involves a chronicinflammation of the sebaceous glands, but the exact cause is
unknown. The diagnosis is usually made in patients com-plaining of vulvar pruritus
who are known to have sebor-rheic dermatitis in the scalp or other hair-bearing
areas of the body. The lesion may mimic other entities such as pso-riasis or
lichen simplex chronicus. The lesions are
pale red toa yellowish pink and may be covered by an oily appearing, scaly
crust. Because this area of the body remains continuallymoist, occasional
exudative lesions include raw “weeping” patches, caused by skin maceration,
which are exacerbated by the patient’s scratching. As with psoriasis, vulvar biopsy isusually not needed when the
diagnosis is made in conjunction with known seborrheic dermatitis in other
hair-bearing areas. Thehistologic features of seborrheic dermatitis are a
combina-tion of those seen in the acanthotic and spongiotic patterns.
Treatment for vulvar dermatitis
involves removing the offending agent, if applicable, initial perineal hygiene
and the use of a 5% solution of aluminum acetate several times a day, followed
by drying. Topical corticosteroid lotions or creams containing a mixture of an
agent that penetrates well, such as betamethasone valerate, in conjunction with
crotamiton, can be used for symptom control. As with LSC, the use of
antipruritic agents as a bedtime dose in the first 10 days to 2 weeks of
treatment frequently helps break the sleep/scratch cycle and allows the lesions
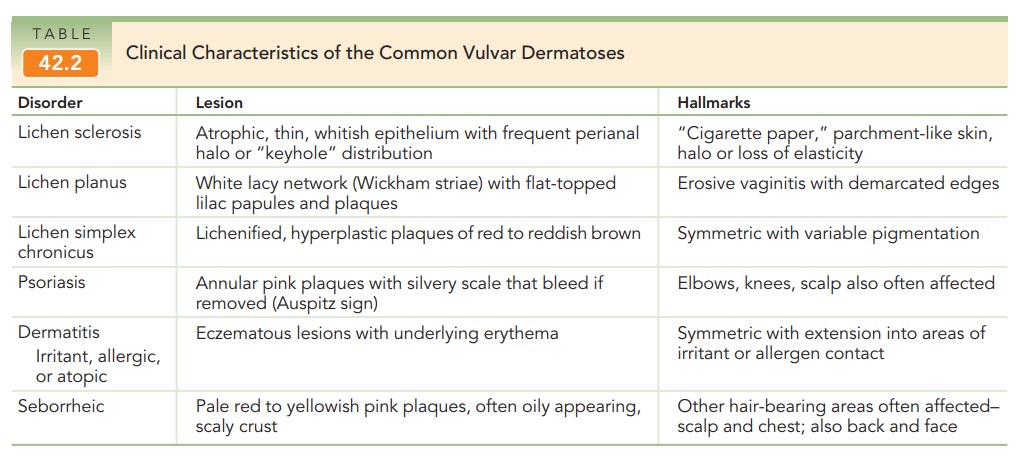
to heal. Table 42.2 summarizes the clinical characteristics of the common
vul-var dermatoses.
Vestibulitis
Vulvar vestibulitis is a condition of unknown etiology. Itinvolves the acute and chronic inflammation of the vestibu-lar glands, which lie just inside the vaginal introitus near the hymeneal ring. The involved glands may be circumferential to include areas near the urethra, but this condition most commonly involves posterolateral vestibular glands between the 4 and 8 o’clock positions (Fig. 42.2). The diagnosis shouldbe suspected in all patients who present with new onset insertional dyspareunia. Patients with this condition frequently com-plain of progressive insertional dyspareunia to the point where they are unable to have intercourse. The history may go on for a few weeks, but most typically involves progres sive worsening over the course of 3 or 4 months. Patients also complain of pain on tampon insertion and at times dur-ing washing or bathing the perineal area.
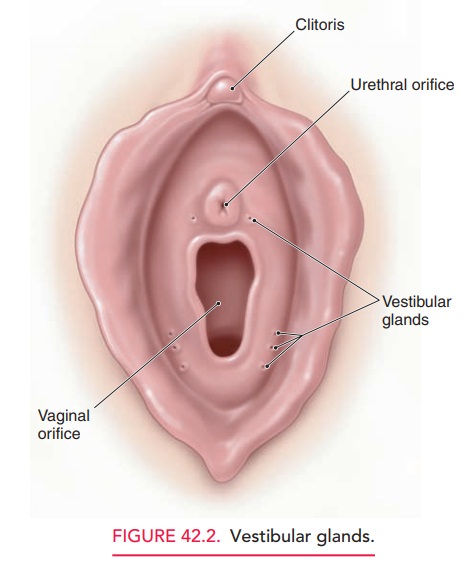
Physical examination is the key
to diagnosis. Because the vestibular glands lie between the folds of the
hymenal ring and the medial aspect of the vulvar vestibule, diagno-sis is
frequently missed when inspection of the perineum does not include these areas:
Once the speculum has been placedin the
vagina, the vestibular gland area becomes impossible to identify. After
carefully inspecting the proper anatomic area,a light touch with a moistened
cotton applicator recreates the pain exactly and allows for quantification of
the pain. In addition, the regions affected are most often evident as small,
reddened, patchy areas.
Because the cause of vestibulitis
is unknown, treatments vary and range from changing or eliminating
environmen-tal factors, temporary sexual abstinence, and application of
cortisone ointments and topical lidocaine (jelly); to more radical treatments
such as surgical excision of the vestibular glands. A combination of treatment
modalities may be nec-essary. Treatment must be individualized, based on the
severity of patient symptoms and the sexual disability.
Some patients may benefit from
low-dose tricyclic medication (amitriptyline and desipramine) or fluoxetine to
help break the cycle of pain. Other limited reports suggest the use of calcium
citrate to change the urine composition by removing oxalic acid crystals. Those
advocating chang-ing the urine chemistry cite evidence to suggest that oxalic
acid crystals are particularly irritating when precipitated in the urine of
patients with high urinary oxalic acid composi-tion. Other modalities include
biofeedback, physical ther-apy with electrical stimulation, or intralesional
injections with triamcinolone and bupivacaine.
Vulvar Lesions
Sebaceous
or inclusion
cysts are caused by inflammatoryblockage of the sebaceous gland ducts and
are small, smooth, nodular masses, usually arising from the inner sur-faces of
the labia minora and majora, that contain cheesy, sebaceous material. They may
be easily excised if their size or position is troublesome.
The round ligament inserts into
the labium majus, car-rying an investment of peritoneum. On occasion,
peritoneal fluid may accumulate therein, causing a cyst of the canalof Nuck or hydrocele. If such cysts reach
symptomaticsize, excision is usually required.
Fibromas (fibromyomas)
arise from the connectivetissue and smooth muscle elements of vulva and vagina
and are usually small and asymptomatic. Sarcomatous change is extremely
uncommon, although edema and degenerative changes may make such lesions
suspicious for malignancy. Treatment is surgical excision when the lesions are
symp-tomatic or with concerns about malignancy. Lipomas appear much like fibromas, are rare, and are also treated
by excision if symptomatic.
Hidradenoma
is a rare lesion arising from the sweatglands of
the vulva. It is almost always benign, is usually found on the inner surface of
the labia majora, and is treated with excision.
Nevi are
benign, usually asymptomatic, pigmentedlesions whose importance is that they
must be distinguished from malignant melanoma, 3% to 4% of which occur on the
external genitalia in females. Biopsy of pigmented vulvar lesions may be
warranted, depending on clinical suspicion.
Related Topics