Chapter: Obstetrics and Gynecology: Vulvar and Vaginal Disease and Neoplasia
Vaginal Disease
VAGINAL DISEASE
Vaginal disease can be classified
into three broad categories: benign, precancerous, and cancerous. There are
impor-tant differences in the management and prognosis of these conditions.
Vaginal
neoplasias are rare and usually occur secondary to cervical or vulvar cancers
that have spread to the vagina from the primary site.
Benign Vaginal Masses
Gartner
duct cysts arise from vestigial remnants of thewolffian or
mesonephric system that course along the outer anterior aspect of the vaginal
canal. These cystic structures are usually small and asymptomatic, but on
occasion they may be larger and symptomatic so that excision is required.
Inclusion
cysts are usually seen on the posterior lowervaginal
surface, resulting from imperfect approximation of childbirth lacerations or
episiotomy. They are lined with stratified squamous epithelium, their content
is usually cheesy, and they may be excised if symptomatic.
Vaginal Intraepithelial Neoplasia (VAIN)
Vaginal
intraepithelial neoplasia (VAIN) can be classi-fied into three
types:
·
VAIN I involves the basal
epithelial layers
·
VAIN 2 involves up to two-thirds
of the vaginal epithelium
·
VAIN 3 involves most of the
vaginal epithelium (carci-noma in situ)
VAIN is most commonly located in
the upper third of the vagina, a finding that may be partially related to its
association with the more common cervical neoplasias. It is estimated that
one-half to two-thirds of all patients with VAIN have had cervical or vulvar
neoplasia.
Patients with VAIN I and II can
be monitored and typically will not require therapy. Many of these patients
have human papillomavirus infection and atrophic change of the vagina. Topical
estrogen therapy may be useful in some women.
VAIN III appears
to occur more commonly in thethird decade of life onward, although its exact
incidence is unknown. One-half to two-thirds of patients with VAIN have a
previous or coexistent neoplasm of the lower genital tract. Approximately 1% to
2% of patients who undergo hysterectomy for CIN III and many patients who
undergo radiation therapy for other gynecologic malig-nancy ultimately develop
VAIN III. This is one of the arguments for yearly Pap smears after
hysterectomy. The importance of VAIN III is its potential for progression to
invasive vaginal carcinoma, as the lesions themselves are usually asymptomatic
and have no intrinsic morbidity.
VAIN III must be differentiated
from other causes of red, ulcerated, or white hyperplastic lesions of the
vagina such as herpes, traumatic lesions, hyperkeratosis associated with chronic
irritation (e.g., from a poorly fit-ting diaphragm), or adenosis. Inspection
and palpation of the vagina are the mainstays of diagnosis, but,
unfortu-nately, this is often done in a cursory fashion during the routine
pelvic examination. Pap smears of the
vaginal epithe-lium can disclose findings that are useful in the diagnosis,
although colposcopy with directed biopsy is the definitive method of diagnosis,
just as it is with CIN.
The goals of treatment of VAIN
III are ablation of the intraepithelial lesion while preserving vaginal depth,
cal-iber, and sexual function. Laser ablation, local excision, and chemical
treatment with 5-fluorouracil cream are all used for limited lesions; total or
partial vaginectomy with appli-cation of a split thickness skin graft is
usually reserved for failure of the previously described treatments. Cure rates
of 80% to 95% may be expected.
Vaginal Cancer
Invasive vaginal cancer accounts
for approximately 1% to 3% of gynecologic malignancies. Squamous cell carcinoma
makes up approximately 80% to 90% of these malignancies, which occur primarily
in women 55 years of age or older. The
remainder of vaginal carcinomas consists of adenocarcinoma of the vagina and
vaginal melanoma.
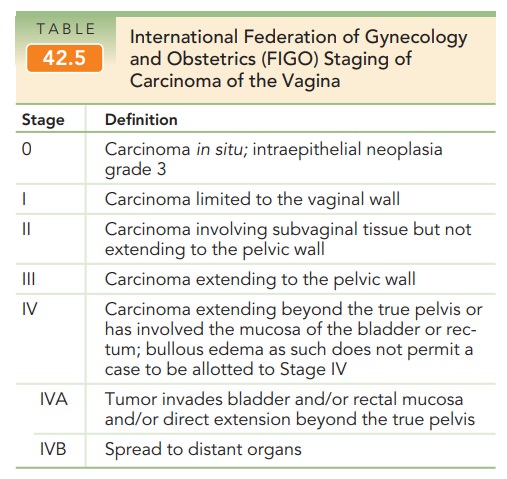
The staging of vaginal carcinoma is nonsurgical (Table 42.5). Radiation therapy is the mainstay of treatment for SCC of the vagina. Radical hysterectomy combined with upper vaginectomy and pelvic lymphadenectomy are used for selected patients.
Upper vaginal lesions and pelvic exenteration and radical
vulvectomy are used for selected patients with lower vaginal lesions involving
the vulva. Most young women with clear cell carcinoma have lesions located in
the upper one-half of the vagina, and wish to maintain ovarian and vaginal
function. Radical hysterectomy with upper vaginectomy combined with pelvic
lymphadenec-tomy is often the primary treatment for these patients, with
radiation therapy following. The overall 5-year survival rate for squamous cell
carcinoma of the vagina is approximately 42%, and for clear cell adenocarcinoma
of the vagina, 78%, with stage I and II patients having the best prognosis.
Melanoma is treated with radical surgery; radiation and chemotherapy have
little efficacy.
Sarcoma
botryoides (or embryonal rhabdomyo-sarcoma) is a rare tumor
that presents as a mass of grape-like polyps protruding from the introitus of
pediatric-age patients. It arises from the undifferentiated mesenchyme of the
lamina propria of the anterior vaginal wall. Bloody discharge is an associated
symptom in these tumors. The tumor spreads locally, although it may have
distant hema-togenous metastases. Combination chemotherapy appears to be
effective, resulting in a marked reduction in tumor size. This permits more
conservative surgery than was performed in the past, preserving as much bowel
and bladder function as possible.
Related Topics