Chapter: Obstetrics and Gynecology: Vulvar and Vaginal Disease and Neoplasia
Vestibulitis - Benign Vulvar Disease
Vestibulitis
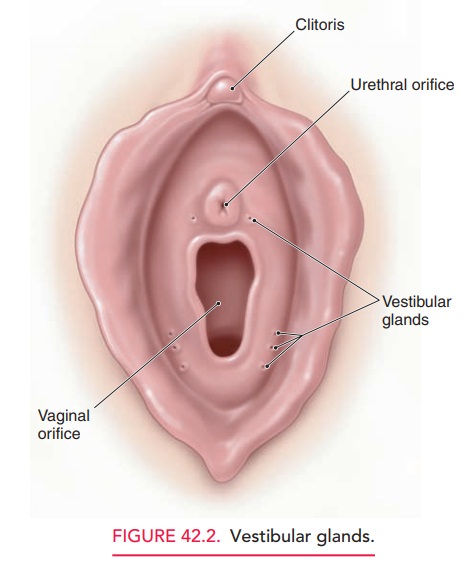
Vulvar vestibulitis is a condition of unknown etiology. Itinvolves the acute and chronic inflammation of the vestibu-lar glands, which lie just inside the vaginal introitus near the hymeneal ring. The involved glands may be circumferential to include areas near the urethra, but this condition most commonly involves posterolateral vestibular glands between the 4 and 8 o’clock positions (Fig. 42.2). The diagnosis shouldbe suspected in all patients who present with new onset insertional dyspareunia. Patients with this condition frequently com-plain of progressive insertional dyspareunia to the point where they are unable to have intercourse. The history may go on for a few weeks, but most typically involves progres sive worsening over the course of 3 or 4 months. Patients also complain of pain on tampon insertion and at times dur-ing washing or bathing the perineal area.
Physical examination is the key
to diagnosis. Because the vestibular glands lie between the folds of the
hymenal ring and the medial aspect of the vulvar vestibule, diagno-sis is
frequently missed when inspection of the perineum does not include these areas:
Once the speculum has been placedin the
vagina, the vestibular gland area becomes impossible to identify. After
carefully inspecting the proper anatomic area,a light touch with a moistened
cotton applicator recreates the pain exactly and allows for quantification of
the pain. In addition, the regions affected are most often evident as small,
reddened, patchy areas.
Because the cause of vestibulitis
is unknown, treatments vary and range from changing or eliminating
environmen-tal factors, temporary sexual abstinence, and application of
cortisone ointments and topical lidocaine (jelly); to more radical treatments
such as surgical excision of the vestibular glands. A combination of treatment
modalities may be nec-essary. Treatment must be individualized, based on the
severity of patient symptoms and the sexual disability.
Some patients may benefit from
low-dose tricyclic medication (amitriptyline and desipramine) or fluoxetine to
help break the cycle of pain. Other limited reports suggest the use of calcium
citrate to change the urine composition by removing oxalic acid crystals. Those
advocating chang-ing the urine chemistry cite evidence to suggest that oxalic
acid crystals are particularly irritating when precipitated in the urine of
patients with high urinary oxalic acid composi-tion. Other modalities include
biofeedback, physical ther-apy with electrical stimulation, or intralesional
injections with triamcinolone and bupivacaine.
Related Topics