Chapter: Obstetrics and Gynecology: Vulvar and Vaginal Disease and Neoplasia
Lichen Planus - Benign Vulvar Disease
Lichen Planus
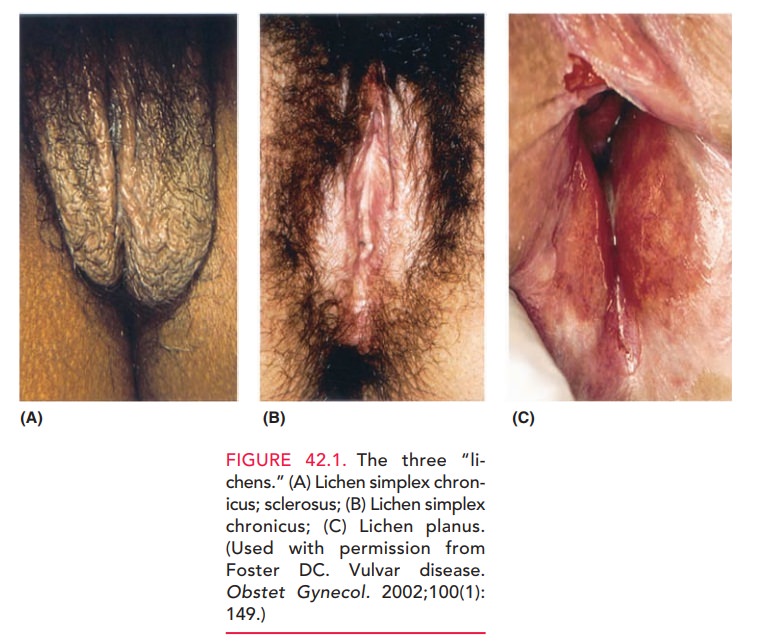
Although lichen planus is usually a desquamative lesion of the vagina,
occasional patients develop lesions on the vulva near the inner aspects of the
labia minora and vulvar vestibule. Patients may have areas of whitish, lacy
bands (Wickham striae) of keratosis near the reddish ulcerated-like lesions
characteristic of the disease (see Figure 42.1C). Typically, complaints include chronic vulvar burning and/or pruritus
and insertional (i.e., entrance) dyspareunia and a pro-fuse vaginal discharge. Because
of the patchiness of thislesion and the concern raised by atypical appearance
of the lesions, biopsy may be warranted to confirm the diagnosis in some
patients. In lichen planus, biopsy shows no atypia. Examination of the vaginal
discharge in these patients fre-quently reveals large numbers of acute
inflammatory cells without significant numbers of bacteria. Accordingly, the
diagnosis most often can be made by the typical history of vaginal/vulvar
burning and/or insertional dyspareunia, coupled with a physical examination
that shows the bright red patchy distribution; and a wet prep that shows large
numbers of white cells. Histologically the epithelium is thinned, and there is
a loss of the rete ridges with a lym-phocytic infiltrate just beneath,
associated with basal cell liquefaction necrosis.
Treatment for lichen planus is
topical steroid prepa-rations similar to those used for lichen simplex
chronicus. This may include the use of intravaginal 1% hydrocorti-sone douches.
Length of treatment for these patients is often shorter than that required to
treat lichen simplex chronicus, although lichen planus is more likely to recur.
Related Topics