Chapter: Basic & Clinical Pharmacology : Nonsteroidal Anti-Inflammatory Drugs, Disease-Modifying Antirheumatic Drugs, Nonopioid Analgesics,& Drugs Used in Gout
Uricosuric Agents
URICOSURIC AGENTS
Probenecid and
sulfinpyrazone are uricosuric drugs employed to decrease the body pool of urate
in patients with tophaceous gout or in those with increasingly frequent gouty
attacks. In a patient who excretes large amounts of uric acid, the uricosuric
agents should not be used.
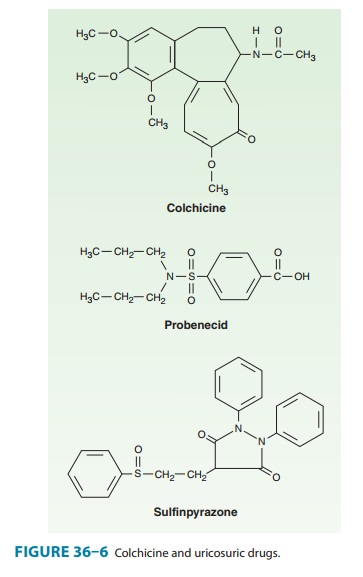
Chemistry
Uricosuric drugs are
organic acids (Figure 36–6) and, as such, act at the anionic transport sites of
the renal tubule . Sulfinpyrazone is a metabolite of an analog of
phenylbutazone.
Pharmacokinetics
Probenecid
is completely reabsorbed by the renal tubules and is metabolized slowly with a
terminal serum half-life of 5–8 hours. Sulfinpyrazone or its active
hydroxylated derivative is rapidly excreted by the kidneys. Even so, the
duration of its effect after oral administration is almost as long as that of
probenecid, which is given once or twice daily.
Pharmacodynamics
Uric acid is freely
filtered at the glomerulus. Like many other weak acids, it is also both
reabsorbed and secreted in the middle seg-ment (S2) of the proximal tubule.
Uricosuric drugs—probenecid, sulfinpyrazone, and large doses of aspirin—affect
these active transport sites so that net reabsorption of uric acid in the
proximal tubule is decreased. Because aspirin in doses of less than 2.6 g daily
causes net retention of uric acid by inhibiting the secretory trans-porter, it
should not be used for analgesia in patients with gout. The secretion of other
weak acids (eg, penicillin) is also reduced by uricosuric agents. Probenecid
was originally developed to pro-long penicillin blood levels.
As the urinary
excretion of uric acid increases, the size of the urate pool decreases,
although the plasma concentration may not be greatly reduced. In patients who
respond favorably, tophaceous deposits of urate are reabsorbed, with relief of
arthritis and remin-eralization of bone. With the ensuing increase in uric acid
excre-tion, a predisposition to the formation of renal stones is augmented
rather than decreased; therefore, the urine volume should be maintained at a
high level, and at least early in treatment, the urine pH should be kept above
6.0 by the administration of alkali.
Indications
Uricosuric therapy
should be initiated in gouty patients with underexcretion of uric acid when
allopurinol or febuxostat is con-traindicated or when tophi are present.
Therapy should not be started until 2–3 weeks after an acute attack.
Adverse Effects
Adverse
effects do not provide a basis for preferring one or the other of the
uricosuric agents. Both of these organic acids cause GI irritation, but
sulfinpyrazone is more active in this regard. A rash may appear after the use
of either compound. Nephrotic syndrome has occurred after the use of
probenecid. Both sulfin-pyrazone and probenecid may rarely cause aplastic
anemia.
Contraindications & Cautions
It is essential to
maintain a large urine volume to minimize the possibility of stone formation.
Dosage
Probenecid is usually
started at a dosage of 0.5 g orally daily in divided doses, progressing to 1 g
daily after 1 week. Sulfinpyrazone is started at a dosage of 200 mg orally
daily, progressing to 400–800 mg daily. It should be given in divided doses
with food to reduce adverse GI effects.
Related Topics