Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Dysfunction
Transsphenoidal Surgery
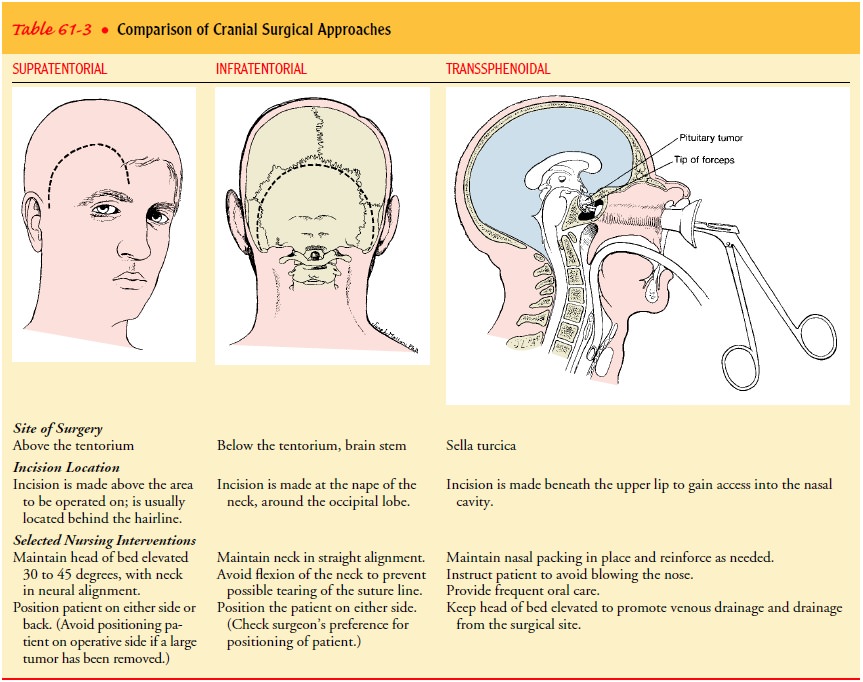
TRANSSPHENOIDAL SURGERY
Tumors
within the sella turcica and small adenomas of the pitu-itary can be removed
through a transsphenoidal approach: an incision is made beneath the upper lip
and entry is then gained successively into the nasal cavity, sphenoidal sinus,
and sella tur-cica (see Table 61-3). Although an otorhinolaryngologist may make
the initial opening, the neurosurgeon completes the open-ing into the
sphenoidal sinus and exposes the floor of the sella. Microsurgical techniques
provide improved illumination, mag-nification, and visualization so that nearby
vital structures can be avoided.
The
transsphenoidal approach offers direct access to the sella with minimal risk of
trauma and hemorrhage (Greenberg, 2001). It avoids many of the risks of
craniotomy, and the postoperative discomfort is similar to that of other
transnasal surgical proce-dures. It may also be used for pituitary ablation
(removal) in pa-tients with disseminated breast or prostatic cancer.
Complications
Manipulation
of the posterior pituitary gland during surgery may produce transient diabetes
insipidus of several days’ duration (Greenberg, 2001). It is treated with
vasopressin but occasionally persists. Other complications include CSF leakage,
visual distur-bances, postoperative meningitis, and SIADH.
Preoperative Evaluation
The
preoperative workup includes a series of endocrine tests, rhi-nologic
evaluation (to assess the status of the sinuses and nasal cavity), and
neuroradiologic studies. Funduscopic examination and visual field
determinations are performed, because the most serious effect of pituitary
tumor is localized pressure on the optic nerve or chiasm. In addition, the
nasopharyngeal secretions are cultured because a sinus infection is a
contraindication to an in-tracranial procedure through this approach.
Corticosteroids may be administered before and after surgery (because the
surgery in-volves removal of the pituitary, the source of adrenocorticotropic
hormone [ACTH] is removed). Antibiotics may or may not be administered
prophylactically (Greenberg, 2001).
Deep
breathing is taught before surgery. The patient is in-structed that following
the surgery he or she will need to avoid vigorous coughing, blowing the nose,
sucking through a straw, or sneezing, because these actions may cause a CSF
leak (Greenberg, 2001; Hickey, 2003).
Postoperative Management
Because
the procedure disrupts the oral and nasal mucous mem-branes, management focuses
on preventing infection and pro-moting healing. Medications include
antimicrobial agents (which are continued until the nasal packing inserted at
the time of surgery is removed), corticosteroids, analgesic agents for
discom-fort, and agents for the control of diabetes insipidus when neces-sary
(Greenberg, 2001).
Nursing Management
Vital signs are measured to monitor hemodynamic,
cardiac, and ventilatory status (Eisenberg & Redick, 1998). Because of the
anatomic proximity of the pituitary gland to the optic chiasm, vi-sual acuity
is assessed at regular intervals. One method is to ask the patient to count the
number of fingers held up by the nurse. Evi-dence of decreasing visual acuity
suggests an expanding hematoma.
The
head of the bed is raised to decrease pressure on the sella turcica and to
promote normal drainage. The patient is cau-tioned against blowing the nose or
engaging in any activity that raises ICP, such as bending over or straining
during urination or defecation.
Intake
and output are measured as a guide to fluid and elec-trolyte replacement. The
urine specific gravity is measured after each voiding (Greenberg, 2001). Daily
weight is monitored. Flu-ids are generally given when nausea ceases, and the
patient then progresses to a regular diet.
The
nasal packing inserted during surgery is checked fre-quently for blood or CSF
drainage. The major discomfort is re-lated to the nasal packing and to mouth
dryness and thirst from mouth-breathing. Oral care is provided every 4 hours or
more fre-quently. Usually, the teeth are not brushed until the incision above
the teeth has healed. The use of warm saline mouth rinses and a cool mist
vaporizer is helpful. Petrolatum is soothing when applied to the lips. A room
humidifier assists in keeping the mu-cous membranes moist. The packing is removed
in 3 to 4 days, and only then can the area around the nares be cleaned with the
prescribed solution to remove crusted blood and moisten the mu-cous membranes
(Hickey, 2003).
Home
care considerations include advising the patient to use a room humidifier to
keep the mucous membranes moist and to soothe irritation. The head of the bed
is elevated for at least 2 weeks after surgery.
Related Topics