Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Dysfunction
Nursing Process: The Patient With an Altered Level of Consciousness
NURSING PROCESS: THE PATIENT WITH AN ALTERED LEVEL OF
CONSCIOUSNESS
Assessment
Where
to begin assessing the patient with an altered LOC de-pends somewhat on each
patient’s circumstances, but clinicians often start by assessing the verbal
response. Determining the pa-tient’s orientation to time, person, and place
assesses verbal re-sponse. The patient is asked to identify the day, date, or
season of the year and to identify where he or she is or to identify the
clinicians, family members, or visitors present. Other questions such as, “Who
is the president?” or “What is the next holiday?”
are
also helpful in determining the patient’s processing of infor-mation in the
environment. (Verbal response cannot be evaluated when the patient is intubated
or has a tracheostomy, and this should be clearly documented.)
Alertness is measured by the patient’s ability to
open the eyes spontaneously or to a stimulus. Patients with severe neurologic
dysfunction cannot do this. The nurse should assess for peri-orbital edema or
trauma, which may prevent the patient from opening the eyes, and document if
this interferes with eye opening.
Motor
response includes spontaneous, purposeful move-ment (eg, the awake patient can
move all four extremities with equal strength), movement only in response to
noxious stimuli (eg, pressure/pain), or abnormal posturing (Bateman, 2001). If
the patient is not responding to commands, the motor response is tested by
applying a painful stimulus (firm but gentle pres-sure) to the nailbed or by
squeezing a muscle. If the patient at-tempts to push away or withdraw, the
response is recorded as purposeful or appropriate (“patient withdraws to
painful stim-uli”). This response is considered purposeful if the patient can
cross from one side of the body to the other in response to nox-ious stimuli.
An inappropriate or nonpurposeful response is random and aimless. Posturing may
be decorticate or decere-brate. The most severe neurologic im-pairment results
in flaccidity. Occasionally, posturing cannot be elicited if the patient has
been given pharmacologic paralyzing agents.
In
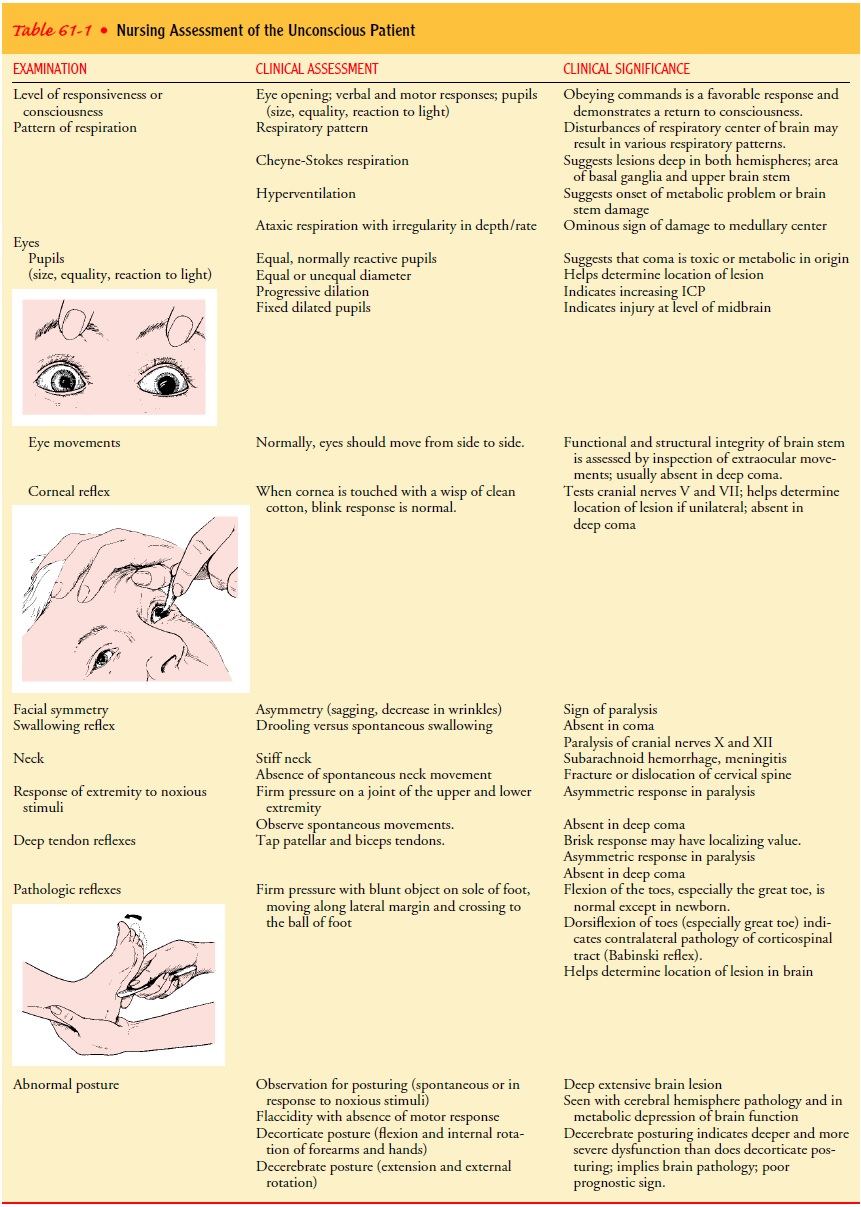
addition to LOC, the nurse monitors parameters such as respiratory status, eye
signs, and reflexes on an ongoing basis. Table 61-1 summarizes the assessment
and the clinical signifi-cance of the findings. Body functions (circulation,
respiration, elimination, fluid and electrolyte balance) are examined in a
sys-tematic and ongoing manner.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the major nursing diagnoses may include the following:
·
Ineffective airway clearance
related to altered level of con-sciousness
·
Risk of injury related to
decreased level of consciousness
·
Deficient fluid volume related
to inability to take in fluids by mouth
·
Impaired oral mucous membranes
related to mouth-breathing, absence of pharyngeal reflex, and altered fluid
intake
·
Risk for impaired skin
integrity related to immobility
·
Impaired tissue integrity of
cornea related to diminished or absent corneal reflex
·
Ineffective thermoregulation
related to damage to hypo-thalamic center
·
Impaired urinary elimination
(incontinence or retention) related to impairment in neurologic sensing and
control
·
Bowel incontinence related to
impairment in neurologic sensing and control and also related to transitions in
nutri-tional delivery methods
·
Disturbed sensory perception
related to neurologic im-pairment
·
Interrupted family processes
related to health crisis
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Based
on the assessment data, potential complications may include:
·
Respiratory distress or
failure
·
Pneumonia
·
Aspiration
·
Pressure ulcer
·
Deep vein thrombosis
Planning and Goals
The
goals of care for the patient with altered LOC include main-tenance of a clear
airway, protection from injury, attainment of fluid volume balance, achievement
of intact oral mucous mem-branes, maintenance of normal skin integrity, absence
of corneal irritation, attainment of effective thermoregulation, and effective urinary
elimination. Additional goals include bowel continence, accurate perception of
environmental stimuli, maintenance of in-tact family or support system, and
absence of complications (Jacobson & Winslow, 2000).
Because the unconscious patient’s protective reflexes are im-paired, the quality of nursing care provided literally may mean the difference between life and death. The nurse must assume re-sponsibility for the patient until the basic reflexes (coughing, blinking, and swallowing) return and the patient becomes con-scious and oriented. Thus, the major nursing goal is to compen-sate for the absence of these protective reflexes.
Nursing Interventions
MAINTAINING THE AIRWAY
The
most important consideration in managing the patient with altered LOC is to
establish an adequate airway and ensure venti-lation. Obstruction of the airway
is a risk because the epiglottis and tongue may relax, occluding the
oropharynx, or the patient may aspirate vomitus or nasopharyngeal secretions.
The accumulation of secretions in the pharynx
presents a se-rious problem. Because the patient cannot swallow and lacks
pharyngeal reflexes, these secretions must be removed to elimi-nate the danger
of aspiration. Elevating the head of the bed to 30 degrees helps prevent
aspiration. Positioning the patient in a lateral or semiprone position will
also help as it permits the jaw and tongue to fall forward, thus promoting
drainage of secretions.
Positioning alone is not always adequate, however.
The pa-tient may require suctioning and oral hygiene. Suctioning is per-formed
to remove secretions from the posterior pharynx and upper trachea. With the
suction off, a whistle-tip catheter is lubricated with a water-soluble
lubricant and inserted to the level of the pos-terior pharynx and upper
trachea. Continuous suction is applied as the catheter is withdrawn using a
twisting motion of the thumb and forefinger. This twisting maneuver prevents
the suctioning end of the catheter from causing irritation, which increases
se-cretions and causes mucosal trauma and bleeding. Before and after
suctioning, the patient is hyperoxygenated and hyperventi-lated to prevent
hypoxia (Hickey, 2003). In addition to these interventions, chest physiotherapy
and postural drainage may be initiated to promote pulmonary hygiene, unless
contraindicated by the patient’s underlying condition. Also, the chest should
be auscultated at least every 8 hours to detect adventitious breath sounds or
absence of breath sounds.
Despite
these measures, or because of the severity of impair-ment, the patient with
altered LOC often requires intubation and mechanical ventilation. Nursing
actions for the mechanically ventilated patient include maintaining the patency
of the endo-tracheal tube or tracheostomy, providing frequent oral care,
mon-itoring arterial blood gas measurements, and maintaining ventilator
settings.
PROTECTING THE PATIENT
For the protection of the patient, padded siderails
are provided and raised at all times. Care should be taken to prevent injury
from invasive lines and equipment, and other potential sources of injury should
be identified (eg, restraints, tight dressings, envi-ronmental irritants, damp
bedding or dressings, tubes and drains).
Protection also encompasses the concept of
protecting the pa-tient’s dignity during altered LOC. Simple measures such as
pro-viding privacy and speaking to the patient during nursing care activities
preserve the patient’s humanity. Not speaking nega-tively about the patient’s
condition or prognosis is also important, because patients in a light coma may
be able to hear. The co-matose patient has an increased need for advocacy, and
it is the nurse’s responsibility to see that these advocacy needs are met
(Elliott & Wright, 1999; Villanueva, 1999).
MAINTAINING FLUID BALANCE AND MANAGING NUTRITIONAL NEEDS
Hydration status is assessed by examining tissue
turgor and mu-cous membranes, assessing intake and output trends, and
analyz-ing laboratory data. Fluid needs are met initially by giving the
required fluids intravenously. However, intravenous solutions (and blood
transfusions) for patients with intracranial conditions must be administered
slowly. If given too rapidly, they may in-crease ICP. The quantity of fluids
administered may be restricted to minimize the possibility of producing
cerebral edema.
If
the patient does not recover quickly and sufficiently enough to take adequate
fluids and calories by mouth, a feeding tube will be inserted for the
administration of fluids and enteral feedings (Day, Stotts, Frankfurt et al.,
2001).
PROVIDING MOUTH CARE
The mouth is inspected for dryness, inflammation,
and crusting. The unconscious patient requires conscientious oral care because
there is a risk of parotitis if the mouth is not kept scrupulously clean. The
mouth is cleansed and rinsed carefully to remove se-cretions and crusts and to
keep the mucous membranes moist. A thin coating of petrolatum on the lips
prevents drying, cracking, and encrustations. If the patient has an
endotracheal tube, the tube should be moved to the opposite side of the mouth
daily to prevent ulceration of the mouth and lips.
MAINTAINING SKIN AND JOINT INTEGRITY
Preventing
skin breakdown requires continuing nursing assess-ment and intervention.
Special attention is given to unconscious patients because they cannot respond
to external stimuli. Assess-ment includes a regular schedule of turning to
avoid pressure, which can cause breakdown and necrosis of the skin. Turning
also provides kinesthetic (sensation of movement), proprioceptive (awareness of
position), and vestibular (equilibrium) stimulation. After turning, the patient
is carefully repositioned to prevent is-chemic necrosis over pressure areas.
Dragging the patient up in bed must be avoided, because this creates a shearing
force and friction on the skin surface.
Maintaining
correct body position is important; equally im-portant is passive exercise of
the extremities to prevent contrac-tures. The use of splints or foam boots aids
in the prevention of footdrop and eliminates the pressure of bedding on the
toes. Trochanter rolls supporting the hip joints keep the legs in proper
alignment. The arms should be in abduction, the fingers lightly flexed, and the
hands in slight supination. The heels of the feet should be assessed for
pressure areas. Specialty beds, such as flu-idized or low-air-loss beds, may be
used to decrease pressure on bony prominences.
PRESERVING CORNEAL INTEGRITY
Some unconscious patients have their eyes open and
have inade-quate or absent corneal reflexes. The cornea is likely to become
irritated or scratched, leading to keratitis and corneal ulcers. The eyes may
be cleansed with cotton balls moistened with sterile nor-mal saline to remove
debris and discharge. If artificial tears are prescribed, they may be instilled
every 2 hours. Periocular edema (swelling around the eyes) often occurs after
cranial surgery. Cold compresses may be prescribed, and care must be exerted to
avoid contact with the cornea. Eye patches should be used cautiously because of
the potential for corneal abrasion from the cornea coming in contact with the
patch.
ACHIEVING THERMOREGULATION
High fever in the unconscious patient may be caused
by infection of the respiratory or urinary tract, drug reactions, or damage to
the hypothalamic temperature-regulating center. A slight eleva-tion of
temperature may be caused by dehydration. The envi-ronment can be adjusted,
depending on the patient’s condition, to promote a normal body temperature. If
body temperature is elevated, a minimum amount of bedding—a sheet or perhaps
only a small drape—is used. The room may be cooled to 18.3°C (65°F). However, if the
patient is elderly and does not have an el-evated temperature, a warmer
environment is needed.
Because
of damage to the heat-regulating center in the brain or severe intracranial
infection, unconscious patients often develop very high temperatures. Such
temperature elevations must be con-trolled because the increased metabolic
demands of the brain can overburden cerebral circulation and oxygenation,
resulting in cere-bral deterioration (Hickey, 2003). Persistent hyperthermia
with no identified clinical source of infection indicates brain stem damage and
a poor prognosis.
Strategies
for reducing fever include:
·
Removing all bedding over the
patient (with the possible ex-ception of a light sheet or small drape)
·
Administering repeated doses
of acetaminophen as pre-scribed
·
Giving a cool sponge bath and
allowing an electric fan to blow over the patient to increase surface cooling
·
Using a hypothermia blanket
Frequent
temperature monitoring is indicated to assess the re-sponse to the therapy and
to prevent an excessive decrease in tem-perature and shivering.
PREVENTING URINARY RETENTION
The
patient with an altered LOC is often incontinent or has uri-nary retention. The
bladder is palpated or scanned at intervals to determine whether urinary
retention is present, because a full bladder may be an overlooked cause of
overflow incontinence. A portable bladder ultrasound instrument is a useful
tool in bladder management and retraining programs (O’Farrell, Vandervoort,
Bisnaire et al., 2001).
If there are signs of urinary retention, initially
an indwelling urinary catheter attached to a closed drainage system is
inserted. A catheter may be inserted during the acute phase of illness to
monitor urinary output. Because catheters are a major factor in causing urinary
tract infection, the patient is observed for fever and cloudy urine. The area
around the urethral orifice is in-spected for drainage. The urinary catheter is
usually removed when the patient has a stable cardiovascular system and if no
di-uresis, sepsis, or voiding dysfunction existed before the onset of coma.
Although many unconscious patients urinate sponta-neously after catheter
removal, the bladder should be palpated or scanned with a portable ultrasound
device periodically for urinary retention (O’Farrell et al., 2001). An
intermittent catheterization program may be initiated to ensure complete emptying
of the bladder at intervals, if indicated.
An external catheter (condom catheter) for the male
patient and absorbent pads for the female patient can be used for the
un-conscious patient who can urinate spontaneously although invol-untarily. As
soon as consciousness is regained, a bladder-training program is initiated. The
incontinent patient is monitored fre-quently for skin irritation and skin
breakdown. Appropriate skin care is implemented to prevent these complications.
PROMOTING BOWEL FUNCTION
The
abdomen is assessed for distention by listening for bowel sounds and measuring
the girth of the abdomen with a tape mea-sure. There is a risk of diarrhea from
infection, antibiotics, and hyperosmolar fluids. Frequent loose stools may also
occur with fecal impaction. Commercial fecal collection bags are available for
patients with fecal incontinence.
Immobility
and lack of dietary fiber may cause constipation. The nurse monitors the number
and consistency of bowel move-ments and performs a rectal examination for signs
of fecal im-paction. Stool softeners may be prescribed and can be administered
with tube feedings. To facilitate bowel emptying, a glycerine sup-pository may
be indicated. The patient may require an enema every other day to empty the lower
colon.
PROVIDING SENSORY STIMULATION
Sensory stimulation is provided at the appropriate
time to help overcome the profound sensory deprivation of the unconscious
patient. Efforts are made to maintain the sense of daily rhythm by keeping the
usual day and night patterns for activity and sleep. The nurse touches and
talks to the patient and encourages fam-ily members and friends to do so.
Communication is extremely important and includes touching the patient and
spending enough time with him or her to become sensitive to his or her needs.
It is also important to avoid making any negative comments about the patient’s
status or prognosis in the patient’s presence.
The
nurse orients the patient to time and place at least once every 8 hours. Sounds
from the patient’s home and workplace may be introduced using a tape recorder.
Family members can read to the patient from a favorite book and may suggest
radio and television programs that the patient previously enjoyed as a means of
enriching the environment and providing familiar input (Hickey, 2003).
When arousing from coma, many patients experience a
period of agitation, indicating that they are becoming more aware of their
surroundings but still cannot react or communicate in an ap-propriate fashion.
Although disturbing for many family members, this is actually a good clinical
sign. At this time, it is necessary to minimize the stimulation to the patient
by limiting background noises, having only one person speak to the patient at a
time, giving the patient a longer period of time to respond, and allow-ing for
frequent rest or quiet times.
When the patient has regained consciousness,
videotaped fam-ily or social events may assist the patient in recognizing
family and friends and allow him or her to experience missed events.
MEETING FAMILIES’ NEEDS
The family of the patient with altered LOC may be
thrown into a sudden state of crisis and go through the process of severe
anx-iety, denial, anger, remorse, grief, and reconciliation. Depending on the
disorder that caused the altered LOC and the extent of the patient’s recovery,
the family may be unprepared for the changes in the cognitive and physical
status of their loved one. If the patient has significant residual deficits,
the family may require considerable time, assistance, and support to come to
terms with these changes. To help family members mobilize their adaptive
capacities, the nurse can reinforce and clarify information about the patient’s
condition, permit the family to be involved in care, and listen to and
encourage ventilation of feelings and concerns while supporting them in their
decision-making process about posthospitalization management and placement
(Hauber & Testani-Dufour, 2000). Families may benefit from participation in
support groups offered through the hospital, rehabilitation fa-cility, or
community organizations.
In some circumstances, the family may need to face
the death of their loved one. The neurologic patient is often pronounced brain
dead before physiologic death occurs. The term brain death describes irreversible loss of all functions of the
entire brain, in-cluding the brain stem. The term may be misleading to the
family because although brain function has ceased, the patient appears to be
alive, with the heart rate and blood pressure sustained by vaso-active
medications, and breathing continues by mechanical ven-tilation. When
discussing a patient who is brain dead with family members, it is important to
use the term “dead”; the term “brain dead” may confuse them (Shewmon, 1998). Chart
61-1 discusses ethical issues related to patients with severe neurologic
damage.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Pneumonia,
aspiration, and respiratory failure are potential com-plications in any patient
who has a depressed LOC and who can-not protect the airway or turn, cough, and
take deep breaths. The longer the period of unconsciousness, the greater the
risk for pul-monary complications.
Vital signs and respiratory function are monitored closely to detect any signs of respiratory failure or distress. Total blood count
and arterial blood gas measurements are assessed to deter-mine whether there
are adequate red blood cells to carry oxygen and whether ventilation is
effective. Chest physiotherapy and suctioning are initiated to prevent
respiratory complications such as pneumonia. If pneumonia develops, cultures
are obtained to identify the organism so that appropriate antibiotics can be
administered.
The
patient with altered LOC is monitored closely for evi-dence of impaired skin
integrity, and strategies to prevent skin breakdown and pressure ulcers are
continued through all phases of care, including hospital, rehabilitation, and
home care. Factors that contribute to impaired skin integrity (eg, incontinence,
in-adequate dietary intake, pressure on bony prominences, edema) are addressed.
If pressure ulcers develop, strategies to promote healing are undertaken. Care
is taken to prevent bacterial conta-mination of pressure ulcers, which may lead
to sepsis and septic shock.
The patient should also be monitored for signs and
symptoms of deep vein thrombosis. Patients who develop deep vein throm-bosis
are at risk for pulmonary embolism. Prophylaxis such as sub-cutaneous heparin
or low-molecular-weight heparin (Fragmin, Orgaran) should be prescribed (Karch,
2002). Thigh-high elas-tic compression stockings or pneumatic compression
stockings should also be prescribed to reduce the risk for clot formation.
Measures to assess for deep vein thrombosis, such as Homans’ sign, may be
clinically unreliable in this population, and the nurse should observe for
redness and swelling in the lower extremities.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Maintains
clear airway and demonstrates appropriate breath sounds
2) Experiences
no injuries
3) Attains/maintains
adequate fluid status
a) Has
no clinical signs or symptoms of dehydration
b) Demonstrates
normal range of serum electrolytes
c) Has
no clinical signs or symptoms of overhydration
4) Attains/maintains
healthy oral mucous membranes
5) Maintains
normal skin integrity
6) Has
no corneal irritation
7) Attains
or maintains thermoregulation
8) Has
no urinary retention
9) Has
no diarrhea or fecal impaction
10) Receives
appropriate sensory stimulation
11) Family
members cope with crisis
a) Verbalize
fears and concerns
b) Participate
in patient’s care and provide sensory stim-ulation by talking and touching
12) Is
free of complications
a) Has
arterial blood gas values within normal range
b) Displays
no signs or symptoms of pneumonia
c) Exhibits
intact skin over pressure areas
d) Does
not develop deep vein thrombosis
Related Topics