Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Dysfunction
Nursing Process: The Patient Undergoing Intracranial Surgery
NURSING PROCESS: THE PATIENT
UNDERGOING INTRACRANIAL SURGERY
Assessment
After
surgery, the frequency of postoperative monitoring is based on the patient’s
clinical status. Assessing respiratory function is essential because even a
small degree of hypoxia can increase cere-bral ischemia. The respiratory rate
and pattern are monitored, and arterial blood gas values are assessed
frequently. Fluctuations in vital signs are carefully monitored and documented
because they indicate increased ICP. The patient’s temperature is mea-sured at
intervals to assess for hyperthermia secondary to damage to the hypothalamus.
Neurologic checks are made frequently to detect increased ICP resulting from
cerebral edema or bleeding. A change in LOC or response to stimuli may be the
first sign of increasing ICP.
The surgical dressing is inspected for evidence of
bleeding and CSF drainage. The nurse must be alert to the development of
com-plications; all assessments are carried out with these problems in mind.
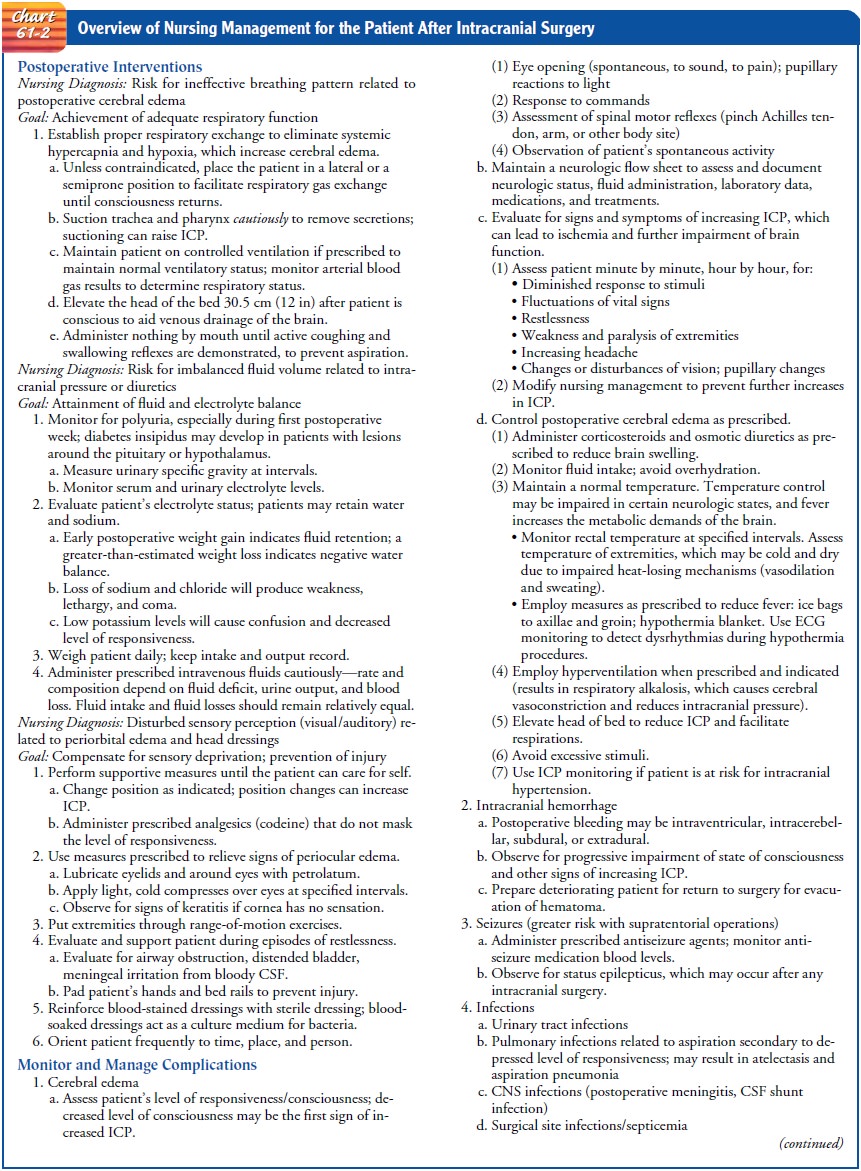
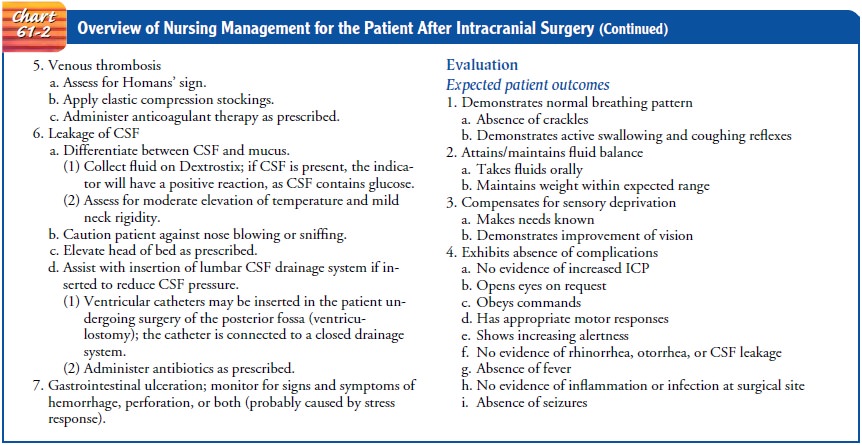
Chart 61-2 provides an overview of the nursing management of the patient after
intracranial surgery. Seizures are a potential com-plication, and any seizure
activity is carefully recorded and reported. Restlessness may occur as the
patient becomes more responsive or may be due to pain, confusion, hypoxia, or
other stimuli.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the patient’s major nursing diag-noses after
intracranial surgery may include the following:
·
Ineffective cerebral tissue
perfusion related to cerebral edema
·
Potential for ineffective
thermoregulation related to dam-age to the hypothalamus, dehydration, and
infection
·
Potential for impaired gas
exchange related to hypoventila-tion, aspiration, and immobility
·
Disturbed sensory perception
related to periorbital edema, head dressing, endotracheal tube, and effects of
ICP
·
Body image disturbance related
to change in appearance or physical disabilities
Other
nursing diagnoses may include impaired communica-tion (aphasia) related to
insult to brain tissue and high risk for impaired skin integrity related to
immobility, pressure, and in-continence. There may be impaired physical
mobility related to a neurologic deficit secondary to the neurosurgical
procedure or to the underlying disorder.
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Potential
complications include:
·
Increased ICP
·
Bleeding and hypovolemic shock
·
Fluid and electrolyte
disturbances
·
Infection
·
Seizures
Planning and Goals
The
major goals for the patient include neurologic homeostasis to improve cerebral
tissue perfusion, adequate thermoregulation, normal ventilation and gas exchange,
ability to cope with sensory deprivation, adaptation to changes in body image,
and absence of complications.
Nursing Interventions
MAINTAINING CEREBRAL TISSUE PERFUSION
Attention to the patient’s respiratory status is
essential because even slight decreases in the oxygen level (hypoxia) can cause
cere-bral ischemia and can affect the clinical course and outcome. The
endotracheal tube is left in place until the patient shows signs of awakening
and has adequate spontaneous ventilation, as evalu-ated clinically and by
arterial blood gas analysis. Secondary brain damage can result from impaired
cerebral oxygenation.
Some degree of cerebral edema occurs after brain
surgery; it tends to peak 24 to 36 hours after surgery, producing decreased
responsiveness on the second postoperative day. The control of cerebral edema
is discussed in the earlier section on management of increased ICP. Nursing
strategies used to control factors that may raise ICP are found earlier in
Nursing Process: The Patient With Increased ICP. Intra-ventricular drainage is
carefully monitored, using strict asepsis when any part of the system is
handled.
Vital signs and neurologic status (LOC and
responsiveness, pupillary and motor responses) are assessed every 15 minutes to
every 1 hour. Extreme head rotation is avoided because this raises ICP. After
supratentorial surgery, the patient is placed on his or her back or side
(unoperated side if a large lesion was removed) with one pillow under the head.
The head of the bed may be elevated 30 degrees, depending on the level of the
ICP and the neurosurgeon’s preference. After posterior fossa (infratentorial)
surgery, the patient is kept flat on one side (off the back) with the head on a
small, firm pillow. The patient may be turned on either side, keeping the neck
in a neutral position. When the patient is being turned, the body should be
turned as a unit to prevent plac-ing strain on the incision and possibly
tearing the sutures. The head of the bed may be elevated slowly as tolerated by
the patient.
The
patient’s position is changed every 2 hours, and skin care is given frequently.
During position changes, care is taken to pre-vent disrupting the ICP
monitoring system. A turning sheet placed under the head to the midthigh makes
it easier to move and turn the patient safely.
REGULATING TEMPERATURE
Moderate temperature elevation can be expected
after intracra-nial surgery because of the reaction to blood at the operative
site or in the subarachnoid space. Injury to the hypothalamic centers that
regulate body temperature can occur during surgery. High fever is treated
vigorously to combat the effect of an elevated tem-perature on brain metabolism
and function.
Nursing interventions include monitoring the patient’s tem-perature and using the following measures to reduce body tem-perature: removing blankets, applying ice bags to axilla and groin areas, using a hypothermia blanket as prescribed, and adminis-tering prescribed medications to reduce fever.
Conversely, hypothermia may be seen after lengthy
neurosur-gical procedures. Therefore, frequent measurements of rectal
temperature are necessary. Rewarming should occur slowly to prevent shivering,
which increases cellular oxygen demands.
IMPROVING GAS EXCHANGE
The
patient undergoing neurosurgery is at risk for impaired gas ex-change and
pulmonary infections because of immobility, immuno-suppression, decreased LOC,
and fluid restriction. Immobility compromises the respiratory system by causing
pooling and sta-sis of secretions in dependent areas and the development of
at-electasis. The patient whose fluid intake is restricted may be more
vulnerable to atelectasis as a result of inability to expectorate thickened
secretions. Pneumonia is frequently seen in neuro-surgical patients, possibly
related to aspiration and restricted mobility.
The
nurse assesses the patient for signs of respiratory infection, which include
temperature elevation, increased pulse rate, and changes in respirations, and
auscultates the lungs for decreased breath sounds and adventitious sounds.
Repositioning the patient every 2 hours will help
to mobilize pulmonary secretions and prevent stasis. When the patient regains
consciousness, additional measures to expand collapsed alveoli can be
instituted, such as yawning, sighing, deep breathing, incentive spirometry, and
coughing (unless contraindicated). If necessary, the oropharynx and trachea are
suctioned to remove secretions that cannot be raised by coughing; however,
coughing and suctioning increase ICP. Therefore, suctioning should be used
cautiously. In-creasing the humidity in the oxygen delivery system may help to
loosen secretions. The nurse and the respiratory therapist work to-gether to
monitor the effects of chest physical therapy.
MANAGING SENSORY DEPRIVATION
Periorbital
edema is a common consequence of intracranial surgery because fluid drains into
the dependent periorbital areas when the patient has been positioned in a prone
position during surgery. A hematoma may form under the scalp and spread down to
the orbit, producing an area of ecchymosis (black eye).
Before
surgery, the patient and family should be informed that one or both eyes may be
edematous temporarily after surgery. After surgery, placing the patient in a
head-up position (if not contraindicated) and applying cold compresses over the
eyes will help reduce the edema. If periorbital edema increases signifi-cantly,
the surgeon is notified because it may indicate that a post-operative clot is
developing or that there is increasing ICP and poor venous drainage. Health
care personnel should announce their presence when entering the room to avoid
startling the pa-tient whose vision is impaired due to periorbital edema or
neu-rologic deficits.
Additional
factors that can affect sensation include a bulky head dressing, the presence
of an endotracheal tube, and effects of increased ICP. The first postoperative
dressing change is usu-ally performed by the neurosurgeon. In the absence of
bleeding or a CSF leak, every effort is made to minimize the size of the head
dressing. If the patient requires an endotracheal tube for mechanical
ventilation, every effort is made to extubate the pa-tient as soon as clinical
signs indicate it is possible. The patient is monitored closely for the effects
of elevated ICP.
ENHANCING SELF-IMAGE
The patient is encouraged to verbalize feelings and
frustrations about any change in appearance. Nursing support is based on the
patient’s reactions and feelings. Factual information may need to be provided
if the patient has misconceptions about puffiness about the face, periorbital
bruising, and hair loss. Attention to grooming, the use of the patient’s own
clothing, and covering the head with a turban (and ultimately a wig until hair
growth occurs) are encouraged. Social interaction with close friends, family,
and hospital personnel may increase the patient’s sense of self-worth.
As the patient assumes more responsibility for
self-care and participates in more activities, a sense of control and personal
competence will develop. The family and social support system can be of
assistance while the patient recovers from surgery.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Complications
that may develop within hours after surgery in-clude increased ICP, bleeding
and hypovolemic shock, altered fluid and electrolyte balance (including water
intoxication), in-fection, and seizures. These complications require close
collabo-ration between the nurse and the surgeon.
Monitoring for Increased ICP and Bleeding
Increased
ICP and bleeding are life-threatening to the patient who has undergone
intracranial neurosurgery. The following must be kept in mind when caring for
all patients who undergo such surgery:
·
An increase in blood pressure
and decrease in pulse with res-piratory failure may indicate increased ICP.
·
An accumulation of blood under
the bone flap (extradural, subdural, intracerebral) may pose a threat to life.
A clot must be suspected in any patient who does not awaken as expected or
whose condition deteriorates. An intracranial hematoma is suspected if the
patient has any new postoper-ative neurologic deficits (especially a dilated
pupil on the operative side). In these events, the patient is returned to the
operating room immediately for evacuation of the clot if indicated.
·
Cerebral edema, infarction,
metabolic disturbances, and hydrocephalus are conditions that may mimic the
clinical manifestations of a clot.
The
patient is monitored closely for indicators of complica-tions, and early signs
and trends in clinical status are reported to the surgeon. Treatments are
initiated promptly, and the nurse as-sists in evaluating the response to
treatment. The nurse also pro-vides support to the patient and family.
Should
signs and symptoms of increased ICP occur, efforts to decrease the ICP are
initiated: alignment of the head in a neutral position without flexion to
promote venous drainage, elevation of the head of the bed to 30 degrees,
administration of mannitol (an osmotic diuretic), and possible administration
of pharmaco-logic paralyzing agents.
Managing Fluid and Electrolyte Disturbances
Fluid
and electrolyte imbalances may occur because of the pa-tient’s underlying
condition and its management or as complica-tions of surgery. Fluid and
electrolyte disturbances can contribute to the development of cerebral edema.
The postoperative fluid regimen depends on the type
of neu-rosurgical procedure and is determined on an individual basis. The
volume and composition of fluids are adjusted according to daily serum
electrolyte values, along with fluid intake and output.
Sodium
retention may occur in the immediate postoperative period. Serum and urine
electrolytes, blood urea nitrogen, blood glucose, weight, and clinical status
are monitored. Intake and output are measured in view of losses associated with
fever, res-piration, and CSF drainage. Fluids may have to be restricted in
patients with cerebral edema.
Oral
fluids are usually resumed after the first 24 hours (Hickey, 2003). The
presence of gag and swallowing reflexes must be checked before initiation of
oral fluids. Some patients with pos-terior fossa tumors may have impaired
swallowing, so fluids may need to be administered by alternative routes. The
patient should be observed for signs and symptoms of nausea and vomiting as the
diet is progressed (Hickey, 2003).
Patients
undergoing surgery for brain tumors often receive large doses of
corticosteroids and thus tend to develop hyper-glycemia. Therefore, serum
glucose levels are measured every 4 hours. These patients are prone to gastric
ulcers, and therefore histamine-2 receptor antagonists (H2
blockers) are prescribed to suppress the secretion of gastric acid. The patient
is monitored for bleeding and assessed for gastric pain.
If
the surgical site is near, or causes edema to, the pituitary gland and
hypothalamus, the patient may develop symptoms of diabetes insipidus, which is
characterized by excessive urinary output. The urine specific gravity is
measured hourly, and fluid intake and output are monitored. Fluid replacement
must com-pensate for urine output, and serum potassium levels must be
monitored.
SIADH,
which results in water retention with hyponatremia and serum hypo-osmolality,
occurs in a wide variety of central nervous system disorders (brain tumor, head
trauma) causing fluid disturbances. Nursing management includes careful intake
and output measurements, specific gravity determinations of urine, and
monitoring of serum and urine electrolyte studies, while following directives
for fluid restriction. SIADH is usually self-limiting.
Preventing Infection
The
patient undergoing neurosurgery is at risk for infection re-lated to the
neurosurgical procedure (brain exposure, bone expo-sure, wound hematomas) and
the presence of intravenous and arterial lines for fluid administration and
monitoring. Risk for in-fection is increased in patients who undergo lengthy
intracranial operations and those with external ventricular drains in place
longer than 48 to 72 hours.
The incision site is monitored for redness,
tenderness, bulging, separation, or foul odor. The dressing is often stained
with blood in the immediate postoperative period. It is important to re-inforce
the dressing with sterile pads so that contamination and infection are avoided.
(Blood is an excellent culture medium for bacteria.) If the dressing is heavily
stained or displaced, this should be reported immediately. (A drain is
sometimes placed in the craniotomy incision to facilitate drainage.)
After
suboccipital surgical procedures, CSF may leak through the incision. This
complication is dangerous because of the pos-sibility of meningitis. Any sudden
discharge of fluid from a cra-nial incision is reported at once because a
massive leak requires direct surgical repair. Attention should be paid to the
patient who complains of a salty taste, because this can be due to CSF
trick-ling down the throat. The patient is advised to avoid coughing, sneezing,
or nose blowing, which may cause CSF leakage by cre-ating pressure on the operative
site.
Aseptic
technique is used when handling dressings, drainage systems, and intravenous
and arterial lines. The patient is moni-tored carefully for signs and symptoms
of infection, and cultures are obtained from the patient with suspected infection.
Appro-priate antibiotics are administered as prescribed.
Other
causes of infection in the patient undergoing intra-cranial surgery are similar
to those in other postoperative patients: pneumonia and urinary tract
infections.
Monitoring for Seizure Activity
Seizures and epilepsy may be complications after
any intracranial neurosurgical procedure. Preventing seizures is essential to
avoid further cerebral edema. Administering the prescribed antiseizure
medication before and immediately after surgery may prevent the development of
seizures in subsequent months and years. Status
epilepticus (prolonged seizures without recovery of consciousnessin the
intervals between seizures) may occur after craniotomy and also may be related
to the development of complications (hematoma, ischemia).
Monitoring and Managing Later Complications
Other
complications may occur during the first 2 weeks or later and may threaten the
patient’s recovery. The most important of these are thromboembolic
complications (deep vein thrombosis, pulmonary embolism), pulmonary and urinary
tract infection, and pressure ulcers (Warbel, Lewicki & Lupica, 1999). Most
of these complications may be avoided with frequent changes of position,
adequate suctioning of secretions, assessment for pul-monary complications,
observation for urinary complications, and skin care.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The
recovery at home of a neurosurgical patient depends on the extent of the
surgical procedure and its success. The patient’s strengths as well as
limitations are explained to the family, along with their part in promoting
recovery. Because administration of antiseizure medication is a priority, the
patient and family are en-couraged to use a check-off system to ensure that the
medication is taken as prescribed.
Usually
no dietary restrictions are required unless another health problem requiring a
special diet exists. Although taking a shower or tub bath is permitted, the
scalp should be kept dry until all the sutures have been removed. A clean scarf
or cap may be worn until a wig or hairpiece is purchased. If skull bone has
been removed, the neurosurgeon may suggest a protective hel-met. After a
craniotomy, the patient may require rehabilitation, depending on the postoperative
level of function. The patient may require physical therapy for residual
weakness and mobil-ity issues. Occupational therapy is consulted to assist with
self-care issues. If the patient is aphasic, speech therapy may be necessary.
Continuing Care
Barring
complications, patients are discharged from the hospital as soon as possible.
Patients with severe motor deficits require ex-tensive physical therapy and
rehabilitation. Those with post-operative cognitive and speech impairments
require psychological evaluation, speech therapy, and rehabilitation. The nurse
works collaboratively with the physician and other health care profes-sionals
during hospitalization and home care to achieve as com-plete a rehabilitation
as possible.
When
tumor, injury, or disease makes the prognosis poor, care is directed toward
making the patient as comfortable as possible. With return of the tumor or
cerebral compression, the patient becomes less alert and aware. Other possible
conse-quences include paralysis, blindness, and seizures. The home care nurse,
hospice nurse, and social worker work with the fam-ily to plan for additional
home health care or hospice services or placement of the patient in an
extended-care facility. The patient and family are encouraged to discuss
end-of-life preferences for care; the patient’s end-of-life preferences must be
respected.
The nurse involved in home and continuing care of patients following cranial surgery needs to remind patients and family members of the need for health promotion and recommended health screening.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Achieves
optimal cerebral tissue perfusion
a) Opens
eyes on request; uses recognizable words, pro-gressing to normal speech
b) Obeys
commands with appropriate motor responses
2) Attains
thermoregulation and normal body temperature
a) Registers
normal body temperature
3) Has
normal gas exchange
a) Has
arterial blood gas values within normal ranges
b) Breathes
easily; lung sounds clear without adventitious sounds
c) Takes
deep breaths and changes position as directed
4) Copes
with sensory deprivation
5) Demonstrates
improving self-concept
a) Pays
attention to grooming
b) Visits
and interacts with others
6) Absence
of complications
a) Exhibits
ICP within normal range
b) Has
minimal bleeding at surgical site; surgical incision is healing without
evidence of infection
c) Shows
fluid balance and electrolyte levels within desired ranges
d) Exhibits
no evidence of seizures
An
overview of care of the patient undergoing intracranial surgery is presented in
Chart 61-2.
Related Topics