Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Dysfunction
Nursing Process: The Patient With Increased ICP
NURSING PROCESS: THE PATIENT WITH INCREASED ICP
Assessment
Initial assessment of the patient with increased
ICP includes ob-taining a history of events leading to the present illness and
other subjective data; it may be necessary to obtain this information from
family or friends. The neurologic examination should be as complete as the
patient’s condition allows. It includes an evaluation of mental status, LOC,
cranial nerve function, cerebellar function (balance and coordination),
reflexes, and motor and sensory func-tion. Because the patient is critically
ill, ongoing assessment willbe more focused, including pupil checks, assessment
of selected cranial nerves, frequent measurements of vital signs and
intra-cranial pressure, and use of the Glasgow Coma Scale. Assessment of the
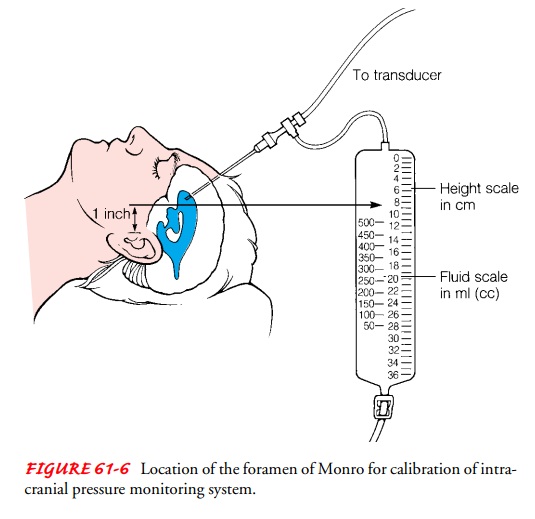
patient with altered LOC is summarized in Table 61-1.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the major nursing diagnoses for pa-tients with
increased ICP include the following:
·
Ineffective airway clearance
related to diminished protective reflexes (cough, gag)
·
Ineffective breathing patterns
related to neurologic dys-function (brain stem compression, structural
displacement)
·
Ineffective cerebral tissue
perfusion related to the effects of increased ICP
·
Deficient fluid volume related
to fluid restriction
·
Risk for infection related to
ICP monitoring system (fiberoptic or intraventricular catheter)
Other
relevant nursing diagnoses are included in the section on caring for patients
with altered LOC.
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based
on the assessment data, potential complications include:
·
Brain stem herniation
·
Diabetes insipidus
·
SIADH
Planning and Goals
The
goals for the patient include maintenance of a patent airway, normalization of
respiration, adequate cerebral tissue perfusion through reduction in ICP,
restoration of fluid balance, absence of infection, and absence of
complications.
Nursing Interventions
MAINTAINING A PATENT AIRWAY
The
patency of the airway is assessed. Secretions obstructing the airway must be
suctioned with care, because transient elevations of ICP occur with suctioning
(Hickey, 2003). The patient is hy-peroxygenated before and after suctioning to
maintain adequate oxygenation. Hypoxia caused by poor oxygenation leads to
cere-bral ischemia and edema. Coughing is discouraged because coughing and
straining also increase ICP. The lung fields are aus-cultated at least every 8
hours to determine the presence of ad-ventitious sounds or any areas of
congestion. Elevating the head of the bed may aid in clearing secretions as
well as improving ve-nous drainage of the brain.
ACHIEVING AN ADEQUATE BREATHING PATTERN
The
patient must be monitored constantly for respiratory irreg-ularities. Increased
pressure on the frontal lobes or deep midline structures may result in
Cheyne-Stokes respirations, whereas pressure in the midbrain may cause
hyperventilation. When the lower portion of the brain stem (the pons and
medulla) is in-volved, respirations become irregular and eventually cease.
If hyperventilation therapy is deemed appropriate
to reduce ICP (by causing cerebral vasoconstriction and a decrease in cere-bral
blood volume), the nurse collaborates with the respiratory therapist in
monitoring PaCO2, which is usually maintained at 35 to 45 mm Hg
(Hickey, 2003).
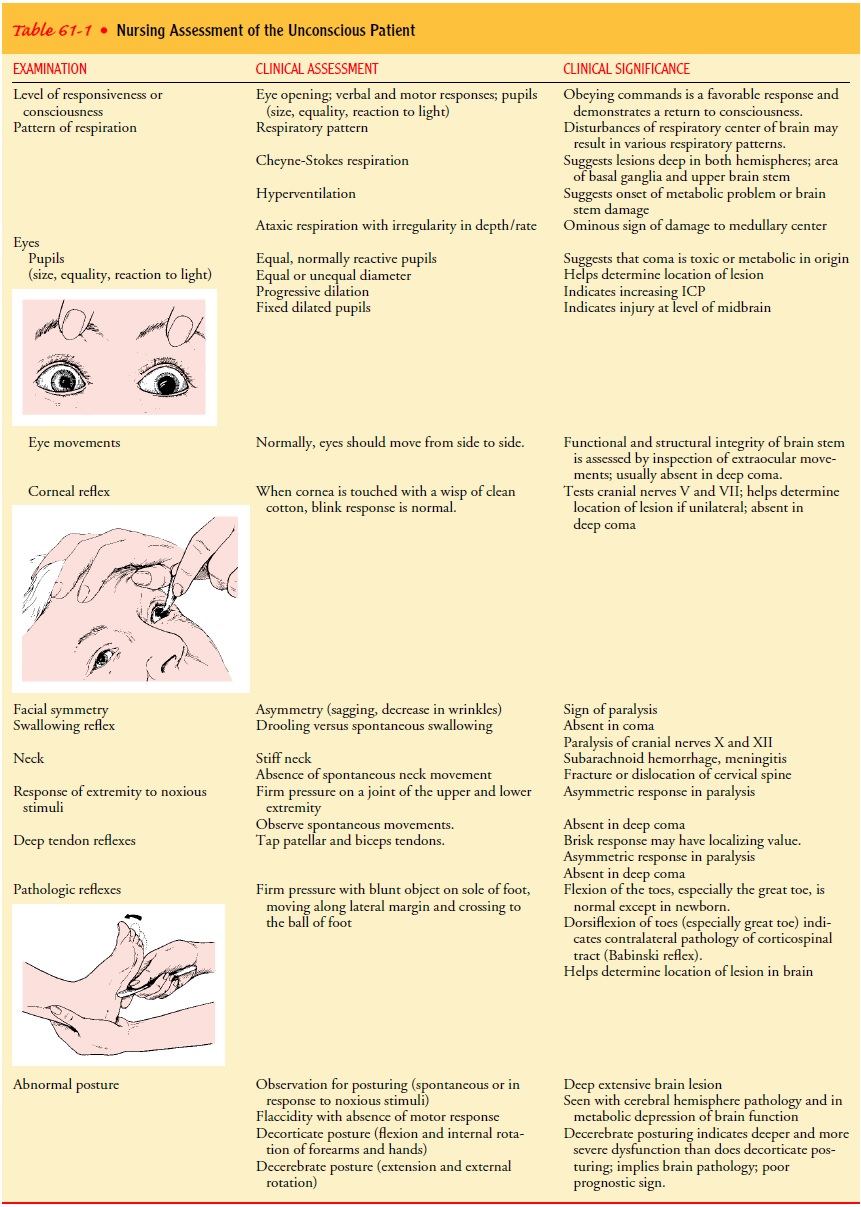
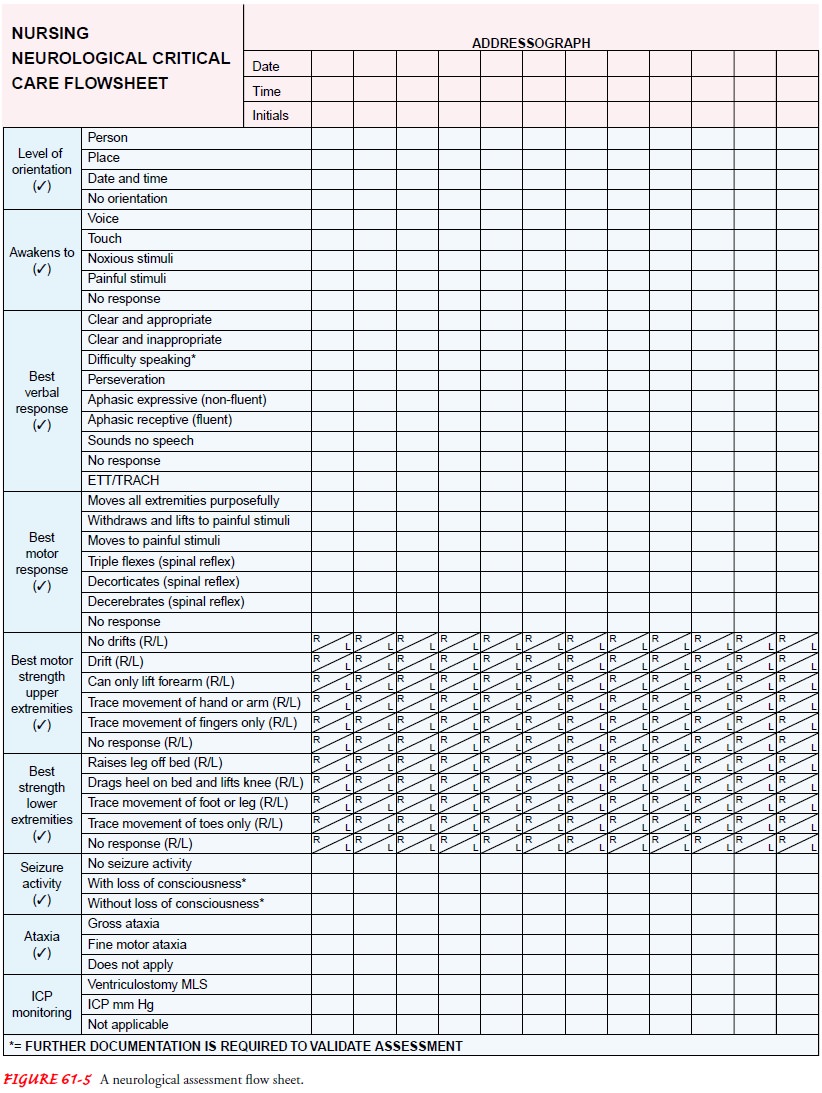
A neurologic observation record (Fig. 61-5) is
maintained, and all observations are made in relation to the patient’s baseline
condition. Repeated assessments of the patient are made (some-times minute by
minute) so that improvement or deterioration may be noted immediately. If the
patient’s condition deteriorates, preparations are made for surgical
intervention.
OPTIMIZING CEREBRAL TISSUE PERFUSION
In
addition to ongoing nursing assessment, strategies are initi-ated to reduce
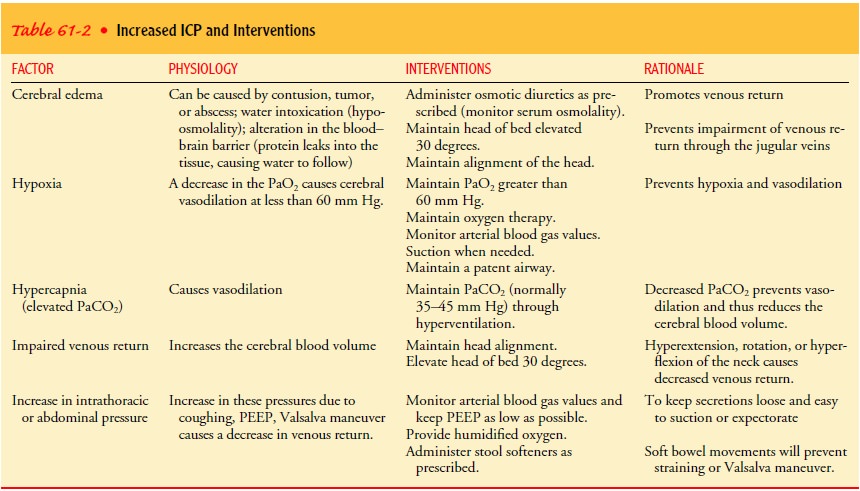
factors contributing to the elevation of ICP (Table 61-2).
Proper
positioning helps to reduce ICP. The head is kept in a neutral (midline)
position, maintained with the use of a cervi-cal collar if necessary, to
promote venous drainage. Elevation of the head is maintained at 0 to 60 degrees
to aid in venous drainage unless otherwise prescribed (Sullivan, 2000). Extreme
rotation of the neck and flexion of the neck are avoided because compression or
distortion of the jugular veins increases ICP. Ex-treme hip flexion is also
avoided because this position causes an increase in intra-abdominal and
intrathoracic pressures, which can produce a rise in ICP. Relatively minor
changes in position may significantly affect ICP (Sullivan, 2000). If monitoring
pa-rameters demonstrate that turning the patient raises ICP, rotat-ing beds,
turning sheets, and holding the patient’s head during turning may minimize the
stimuli that increase ICP.
The
Valsalva maneuver, which can be produced by straining at defecation or even
moving in bed, raises ICP and is to be avoided. Stool softeners may be
prescribed. If the patient is alert and able to eat, a diet high in fiber may
be indicated. Abdominal disten-tion, which increases intra-abdominal and
intrathoracic pressure and ICP, should be noted. Enemas and cathartics are
avoided if possible. When moving or being turned in bed, the patient can be
instructed to exhale (which opens the glottis) to avoid the Valsalva maneuver.
Mechanical
ventilation presents unique problems for the pa-tient with increased ICP.
Before suctioning, the patient should be preoxygenated and hyperventilated
using 100% oxygen on the ventilator (Hickey, 2003). Suctioning should not last
longer than 15 seconds. High levels of positive end-expiratory pressure are
avoided because they may decrease venous return to the heart and decrease
venous drainage from the brain through increased intra-thoracic pressure
(Hickey, 2003).
Activities
that raise ICP, as indicated by changes in wave-forms, should be avoided if
possible. Spacing nursing interven-tions may prevent transient increases in
ICP. During nursing interventions, the ICP should not rise above 25 mm Hg and
should return to baseline levels within 5 minutes. Patients with increased ICP
should not demonstrate a significant increase in pressure or change in the ICP
waveform. Patients with the po-tential for a significant increase in ICP should
receive sedation or “paralyzation” before initiation of many nursing activities
(Hickey, 2003; McConnell, 2001).
Emotional
stress and frequent arousal from sleep are avoided. A calm atmosphere is
maintained. Environmental stimuli (noise, conversation) should be minimal.
Isometric muscle contractions are also contraindicated because they raise the
systemic blood pressure and hence the ICP.
MAINTAINING NEGATIVE FLUID BALANCE
The administration of various osmotic and loop diuretics is part of the treatment protocol to reduce ICP. Corticosteroids are used to reduce cerebral edema, and fluids may be restricted. All of these treatment modalities promote dehydration.
Skin
turgor, mucous membranes, and serum and urine os-molality are monitored to
assess fluid status. If fluids are given intravenously, the nurse ensures they
are administered at a slow to moderate rate with an intravenous infusion pump
to prevent too-rapid administration and avoid overhydration. For the patient
receiving mannitol, the nurse observes for the possible development of heart
failure and pulmonary edema, because the intent of treatment is for fluid to
shift from the intracellular compartment to the intravascular system, thus
controlling cere-bral edema.
For patients undergoing dehydrating procedures,
vital signs, including blood pressure, must be monitored to assess fluid
vol-ume status. An indwelling urinary catheter is inserted to permit assessment
of renal function and fluid status. During the acute phase, urine output should
be monitored every hour. An output greater than 200 mL/hr for 2 consecutive
hours may indicate the onset of diabetes insipidus (Cruz, 1998). These patients
also need careful oral hygiene because mouth dryness is associated with
de-hydration. Frequently rinsing the mouth, lubricating the lips, and removing
encrustations relieve dryness and promote comfort.
PREVENTING INFECTION
Risk
for infection is greatest when ICP is monitored with an in-traventricular
catheter. Most health care facilities have written protocols for managing these
systems and maintaining their sterility; strict adherence to them is essential.
The dressing over the ventricular catheter must be
kept dry be-cause a wet dressing is conducive to bacterial growth. Aseptic
technique must be used when managing the system and changing the ventricular
drainage bag. The drainage system is also checkedfor loose connections because
they cause leakage and contamina-tion of the CSF as well as inaccurate readings
of ICP. The nurse should observe the character of the CSF drainage and report
ob-servations of increasing cloudiness or blood. The patient is mon-itored for
signs and symptoms of meningitis: fever, chills, nuchal (neck) rigidity, and
increasing or persisting headache.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
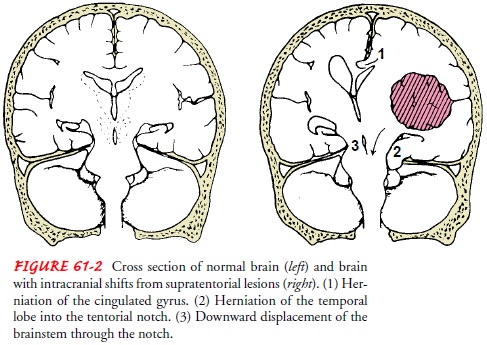
The primary complication of increased ICP is brain
herniation resulting in death (see Fig. 61-2). Nursing management focuses on
detecting early signs of increasing ICP because medical inter-ventions are
usually ineffective once later signs develop. Frequent neurologic assessment
and documentation and analysis of trends will reveal the subtle changes that
may herald rising ICP.
Detecting Early Indications of Increasing ICP
The
nurse assesses for and immediately reports any of the fol-lowing early signs or
symptoms of increasing ICP:
·
Disorientation, restlessness,
increased respiratory effort, pur-poseless movements, and mental confusion;
these are early clinical indications of rising ICP because the brain cells
re-sponsible for cognition are extremely sensitive to decreased oxygenation
·
Pupillary changes and impaired
extraocular movements; these occur as the increasing pressure displaces the
brain against the oculomotor and optic nerves (cranial nerves II, III, IV, and
VI) arising from the midbrain and brain stem
·
Weakness in one extremity or
on one side of the body; this occurs as increasing ICP compresses the pyramidal
tracts
·
Headache that is constant,
increasing in intensity, and ag-gravated by movement or straining; this occurs
as increasing ICP causes pressure and stretching of venous and arterial vessels
in the base of the brain
Detecting Later Signs of Increased ICP
As
ICP rises, the patient’s condition worsens, as manifested by the following
later signs and symptoms:
·
LOC continues to deteriorate
until the patient is comatose.
·
The pulse rate and respiratory
rate decrease or become er-ratic, and the blood pressure and temperature rise.
The pulse pressure (the difference between the systolic and the diastolic
pressures) widens. The pulse fluctuates rapidly, varying from bradycardia to
tachycardia.
·
Altered respiratory patterns
develop, including Cheyne-Stokes breathing (rhythmic waxing and waning of rate
and depth of respirations alternating with brief periods of apnea) and ataxic
breathing (irregular breathing with a random se-quence of deep and shallow
breaths).
·
Projectile vomiting may occur
with increased pressure on the reflex center in the medulla.
·
Hemiplegia or decorticate or
decerebrate posturing may de-velop as pressure on the brain stem increases.
Bilateral flac-cidity occurs before death.
·
Loss of brain stem reflexes,
including pupillary, corneal, gag, and swallowing reflexes, is an ominous sign.
Monitoring ICP
Because clinical assessment is not always a
reliable guide in rec-ognizing increased ICP, especially in comatose patients,
ICP mon-itoring is an essential part of management (Hickey, 2003). ICP is
monitored closely for continuous elevation or significant increase over
baseline. The trend of ICP measurements over time is an im-portant indication of
the patient’s underlying status. Vital signs are assessed when the increase in
ICP is noted.
Strict
aseptic technique is used when handling any part of the monitoring system. The
insertion site is inspected for signs of infection. Temperature, pulse, and respirations
are closely mon-itored for systemic signs of infection. All connections and
stop-cocks are checked for leaks, because even small leaks can distort pressure
readings.
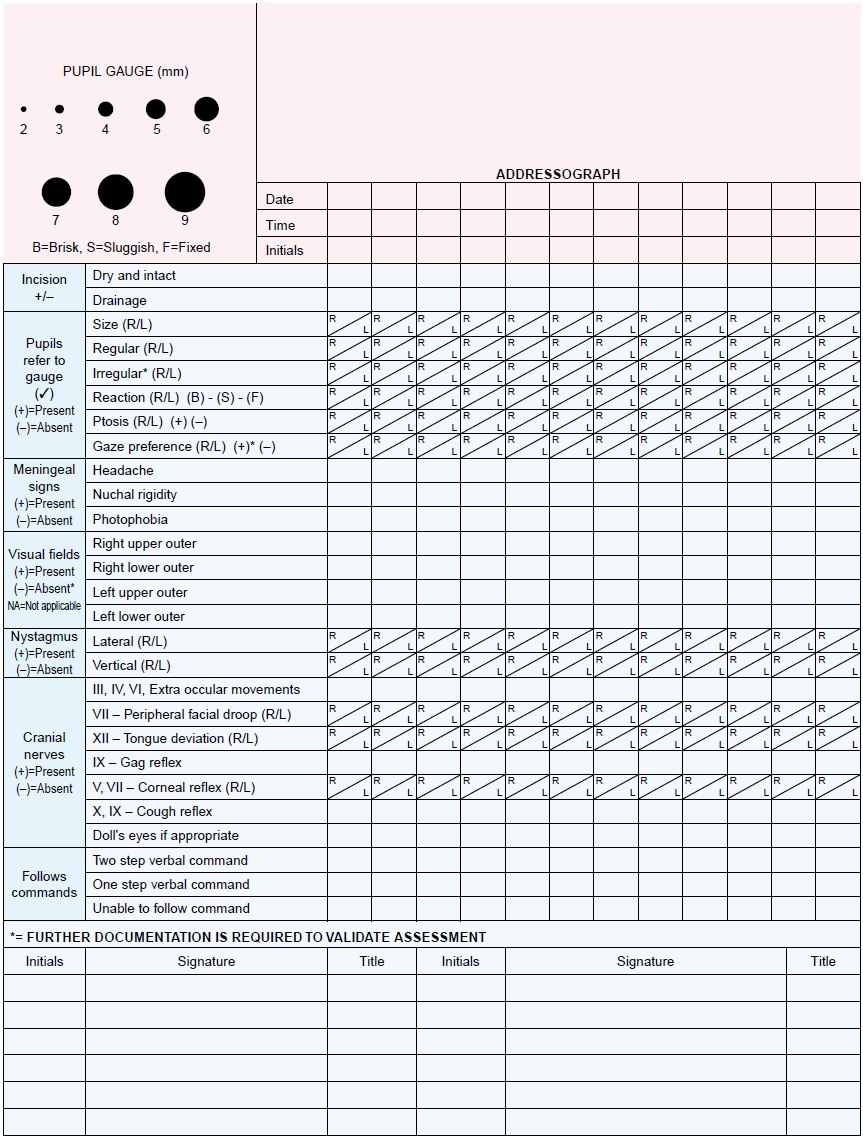
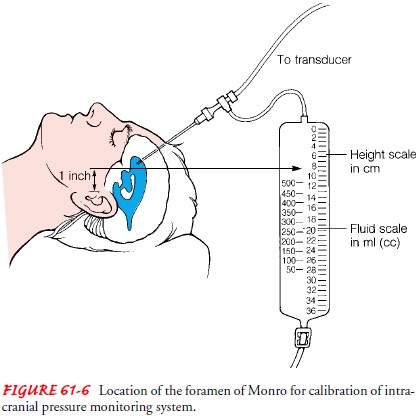
When
ICP is monitored with a fluid system, the transducer is calibrated at a
particular reference point, usually 2.5 cm (1 in) above the ear with the
patient in the supine position; this point corresponds to the level of the
foramen of Monro (Fig. 61-6). (CSF pressure readings depend on the patient’s
position.) For subsequent pressure readings, the head should be in the same
po-sition relative to the transducer. Fiberoptic catheters are cali-brated
before insertion and do not require further referencing; they do not require
the head of the bed to be at a specific position to obtain an accurate reading.
Whenever technology is associated with patient
management, the nurse must be certain that the technology is functioning
prop-erly. The most important concern, however, must be the patient who is
attached to the technology. The patient and family must be informed about the
technology and the goals of its use. The pa-tient’s response is monitored and
appropriate comfort measures are implemented to ensure that the patient’s
stress is minimized.
ICP measurement is only one parameter: repeated neurologic checks and clinical examinations remain important measures. As tute observation, comparison of findings with previous observa-tions, and interventions can assist in preventing life-threatening ICP elevations.
Monitoring for Secondary Complications
The nurse also assesses for complications of
increased ICP, in-cluding diabetes insipidus and SIADH (see Chaps. 14 and 42).
Urine output should be monitored closely. Diabetes insipidus re-quires fluid
and electrolyte replacement, along with the adminis-tration of vasopressin, to
replace and slow the urine output. Serum electrolyte levels should be monitored
for imbalances. SIADH re-quires fluid restriction and monitoring of serum
electrolyte levels.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Maintains
patent airway
2) Attains
optimal breathing pattern
a) Breathes
in a regular pattern
b) Attains
or maintains arterial blood gas values within acceptable range
3) Demonstrates
optimal cerebral tissue perfusion
a) Increasingly
oriented to time, place, and person
b) Follows
verbal commands; answers questions correctly
4) Attains
desired fluid balance
a) Maintains
fluid restriction
b) Demonstrates
serum and urine osmolality values within acceptable range
5) Has
no signs or symptoms of infection
a) Has
no fever
b) Shows
no signs of infection at arterial, intravenous, and urinary catheter sites
c) Has
no purulent drainage from invasive intracranial monitoring device
6) Absence
of complications
a) Has
ICP values that remain within normal limits
b) Demonstrates
urine output and serum electrolyte levels within acceptable limits
Related Topics