Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Dysfunction
Intracranial Surgery
Intracranial Surgery
A craniotomy involves opening the skull surgically
to gain access to intracranial structures. This procedure is performed to
remove a tumor, relieve elevated ICP, evacuate a blood clot, and control
hemorrhage. The surgeon cuts the skull to create a bony flap, which can be
repositioned after surgery and held in place by periosteal or wire sutures. One
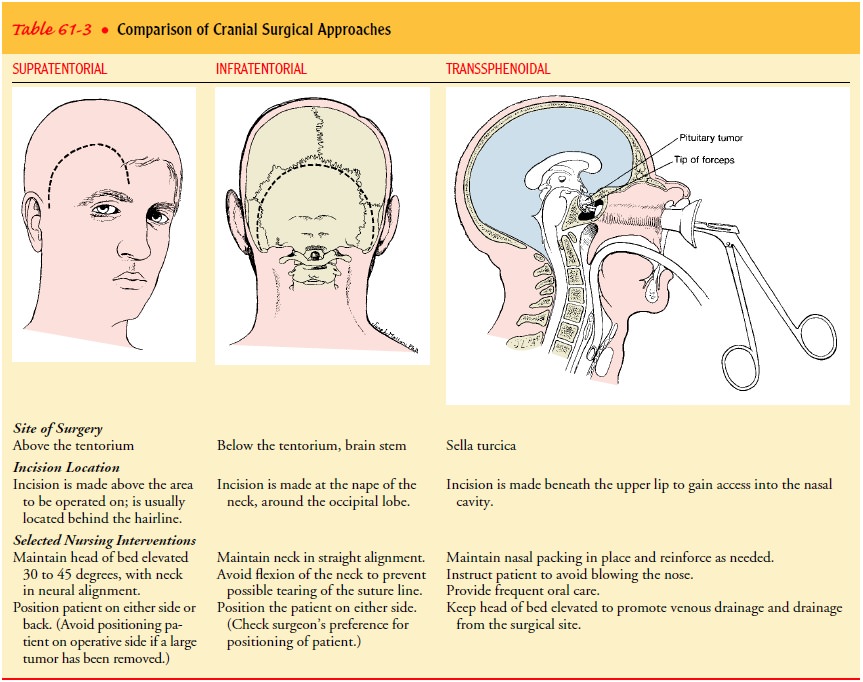
of two approaches through the skull is used: (1) above the tentorium (supratentorial craniotomy)
into the supra-tentorial compartment, or (2) below the tentorium into the
in-fratentorial (posterior fossa) compartment. A transsphenoidal approach through the mouth and nasal sinuses is
used to gain access to the pituitary gland. Table 61-3 compares the three
dif-ferent surgical approaches: supratentorial, infratentorial, and
trans-sphenoidal.
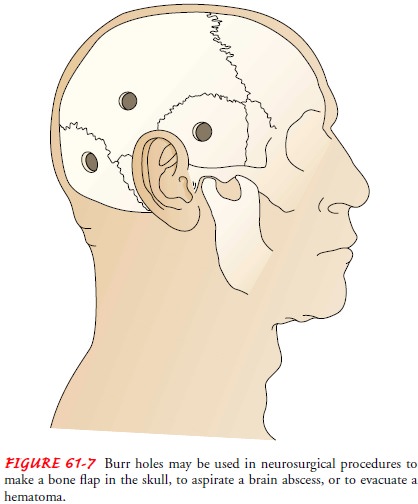
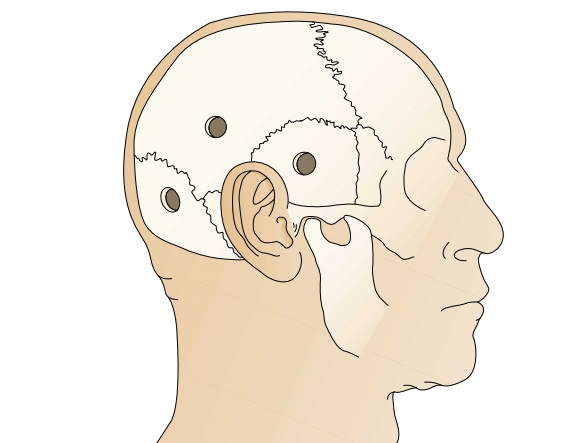
Alternatively, intracranial structures may be
approached through burr holes (Fig. 61-7), which are circular openings made in
the skull by either a hand drill or an automatic craniotome (which has a
self-controlled system to stop the drill when the bone is penetrated). Burr
holes are made for exploration or diagnosis. They may be used to determine the
presence of cerebral swelling and injury and the size and position of the
ventricles. They are also a means of evacuating an intracranial hematoma or
abscess and for making a bone flap in the skull and allowing access to the
ventricles for decompression, ventriculography, or shunting pro-cedures. Other
cranial procedures include craniectomy
(excision of a portion of the skull) and cranioplasty (repair of a cranial
de-fect using a plastic or metal plate).
Preoperative Management
Preoperative diagnostic procedures may include CT
scanning to demonstrate the lesion and show the degree of surrounding brain
edema, the ventricular size, and the displacement. MRI provides information
similar to that of the CT scan and examines the le-sion in other planes
(Tornqvist, 2001). Cerebral angiography may be used to study the tumor’s blood
supply or give informa-tion about vascular lesions. Transcranial Doppler flow
studies are used to evaluate the blood flow of intracranial blood vessels.
Most patients are placed on an antiseizure medication such as phenytoin (Dilantin) or a phenytoin metabolite (Cerebyx) before surgery to reduce the risk of postoperative seizures (paroxysmal transient disturbances of the brain resulting from a discharge of abnormal electrical activity) (Hickey, 2003; Karch, 2002).
Before surgery, corticosteroids such as
dexamethasone (Decadron) may be administered to reduce cerebral edema. Fluids
may be re-stricted. A hyperosmotic agent (mannitol) and a diuretic agent such
as furosemide (Lasix) may be given intravenously immedi-ately before and
sometimes during surgery if the patient tends to retain fluid, as do many who
have intracranial dysfunction. The patient may be given antibiotics if there is
a chance of cerebral contamination; diazepam may be prescribed before surgery
to allay anxiety.
Preoperative Nursing Management
The preoperative assessment serves as a baseline
against which postoperative status and recovery are compared. This assessment
includes evaluating LOC and responsiveness to stimuli and iden-tifying any
neurologic deficits, such as paralysis, visual dysfunc-tion, alterations in
personality or speech, and bladder and bowel disorders. Distal and proximal
motor strength in both upper and lower extremities is recorded using the
5-point scale.
The patient’s and family’s understanding of and
reactions to the anticipated surgical procedure and its possible sequelae are
as-sessed, as is the availability of support systems for the patient and
family. Adequate preparation for surgery, with attention to the patient’s
physical and emotional status, can reduce the risk for anxiety, fear, and
postoperative complications. The patient is as-sessed for neurologic deficits
and their potential impact after surgery. If there are motor deficits or
weakness or paralysis of the arms or legs, trochanter rolls are applied to the
extremities and the feet are positioned against a footboard. A patient who can
am-bulate is encouraged to do so. If the patient is aphasic, writing materials
or picture and word cards showing the bedpan, glass of water, blanket, and
other frequently used items may help improve communication.
Preparation of the patient and family includes
providing in-formation about what to expect during and after surgery. The
surgical site is shaved immediately before surgery (usually in the operating
room) so that any resultant superficial abrasions do not have time to become
infected. An indwelling urinary catheter is inserted in the operating room to
drain the bladder during the administration of diuretics and to permit urinary
output to be monitored. The patient may have a central and arterial line placed
for fluid administration and monitoring of pressures after surgery. The large
head dressing applied after surgery may impair hearing temporarily. Vision may
be limited if the eyes are swollen shut. If a tracheostomy or endotracheal tube
is in place, the patient will be unable to speak until the tube is removed, so
an alterna-tive method of communication should be established.
An altered cognitive state may make the patient
unaware of the impending surgery. Even so, encouragement and attention to the
patient’s needs are necessary. Whatever the state of awareness of the patient,
the family needs reassurance and support because they recognize the seriousness
of brain surgery.
Postoperative Management
Postoperatively,
an arterial line and a central venous pressure line may be in place to monitor
and manage blood pressure and cen-tral venous pressure. The patient may be
intubated and may re-ceive supplemental oxygen therapy. Ongoing postoperative
management is aimed at detecting and reducing cerebral edema, relieving pain
and preventing seizures, and monitoring ICP.
REDUCING CEREBRAL EDEMA
Medications
to reduce cerebral edema include mannitol, which increases serum osmolality and
draws free water from areas of the brain (with an intact blood–brain barrier).
The fluid is then ex-creted by osmotic diuresis. Dexamethasone (Decadron) may
be administered intravenously every 6 hours for 24 to 72 hours; the route is switched
to oral as soon as possible and dosage is tapered over 5 to 7 days (Karch,
2002).
RELIEVING PAIN AND PREVENTING SEIZURES
Acetaminophen
is usually prescribed for temperature exceeding 99.6°F (37.5°C) and for pain.
Commonly, the patient has a headache after a craniotomy, usually as a result of
the scalp nerves being stretched and irritated during surgery. Codeine, given
par-enterally, is often sufficient to relieve headache. Morphine sulfate may
also be used in the management of postoperative pain in the craniotomy patient
(Leith, 1998).
Antiseizure
medication (phenytoin, diazepam) is prescribed for patients who have undergone
supratentorial craniotomy be-cause of the high risk of seizures after
supratentorial neurosurgical procedures. Serum levels are monitored to keep the
medications within the therapeutic range.
MONITORING ICP
A ventricular catheter or other type of drain
frequently is inserted in patients undergoing intracranial surgery. The
catheter is con-nected to an external drainage system. The patency of the
catheter is noted by the pulsations of the fluid in the tubing. The ICP can be
assessed using a stopcock attached to the pressure tubing and transducer. The
ICP is measured by turning the three-way stop-cock to the appropriate position
(Hickey, 2003). Care is required to ensure that the system is tight at all
connections and that the stopcock is in the proper position to avoid drainage
of CSF; col-lapse of the ventricles and brain herniation may result if fluid is
removed too rapidly (Hickey, 2003). The catheter is removed when the
ventricular pressure is normal and stable. The neuro-surgeon must be notified
if the catheter appears to be obstructed.
Related Topics