Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Dysfunction
The Epilepsies
THE EPILEPSIES
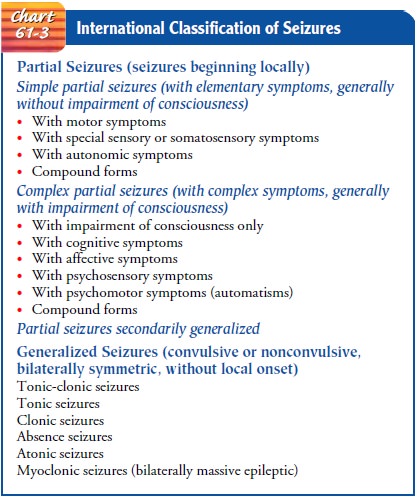
Epilepsy
is a group of syndromes
characterized by recurringseizures. Epileptic syndromes are classified by
specific patterns of clinical features, including age of onset, family history,
and seizure type (Schachter, 2001). Types of epilepsies are differentiated by
how the seizure activity manifests (see Chart 61-3), the most common syndromes
being those with generalized seizures and those with partial-onset seizures.
Epilepsy can be primary (idio-pathic) or secondary, when the cause is known and
the epilepsy is a symptom of another underlying condition such as a brain tumor
(Schachter, 2001).
An estimated 2 to 4 million people in the United States have epilepsy (1 in 100 adults is affected), and onset occurs before the age of 20 years in greater than 75% of patients (Schacter, 2001). The improved treatment of cerebrovascular disorders, head in-juries, brain tumors, meningitis, and encephalitis has increased the number of patients at risk for seizures following recovery from these conditions (Berges et al., 2000). Also, advances in EEG have aided in the diagnosis of epilepsy. The general public has been educated about epilepsy, which has reduced the stigma as-sociated with it; as a result, more people are willing to acknowl-edge the diagnosis.
Although there is evidence that susceptibility to
some types of epilepsy may be inherited, the cause of seizures in many people
is unknown. Epilepsy can follow birth trauma, asphyxia neonatorum, head
injuries, some infectious diseases (bacterial, viral, parasitic), toxicity
(carbon monoxide and lead poisoning), circu-latory problems, fever, metabolic
and nutritional disorders, and drug or alcohol intoxication (Schachter, 2001).
It is also associ-ated with brain tumors, abscesses, and congenital
malformations. In most cases of epilepsy, the cause is unknown (idiopathic).
Pathophysiology
Messages
from the body are carried by the neurons (nerve cells) of the brain by means of
discharges of electrochemical energy that sweep along them. These impulses
occur in bursts whenever a nerve cell has a task to perform. Sometimes, these
cells or groups of cells continue firing after a task is finished. During the
period of unwanted discharges, parts of the body controlled by the er-rant
cells may perform erratically. Resultant dysfunction ranges from mild to
incapacitating and often causes unconsciousness (Greenberg, 2001; Hickey,
2003). When these uncontrolled, ab-normal discharges occur repeatedly, a person
is said to have an epileptic syndrome (Schachter, 2001).
Epilepsy
is not associated with intellectual level. People with epilepsy without other
brain or nervous system disabilities fall within the same intelligence ranges
as the overall population. Epilepsy is not synonymous with mental retardation
or illness. Many who are developmentally disabled because of serious
neu-rologic damage, however, have epilepsy as well.
Clinical Manifestations
Depending on the location of the discharging
neurons, seizures may range from a simple staring episode to prolonged
convulsive movements with loss of consciousness. Seizures have been classi-fied
according to the area of the brain involved and have been identified as
partial, generalized, and unclassified (Greenberg, 2001; Hickey, 2003). Partial
seizures are focal in origin and af-fect only part of the brain. Generalized
seizures are nonspecific in origin and affect the entire brain simultaneously.
Unclassified seizures are so termed because of incomplete data.
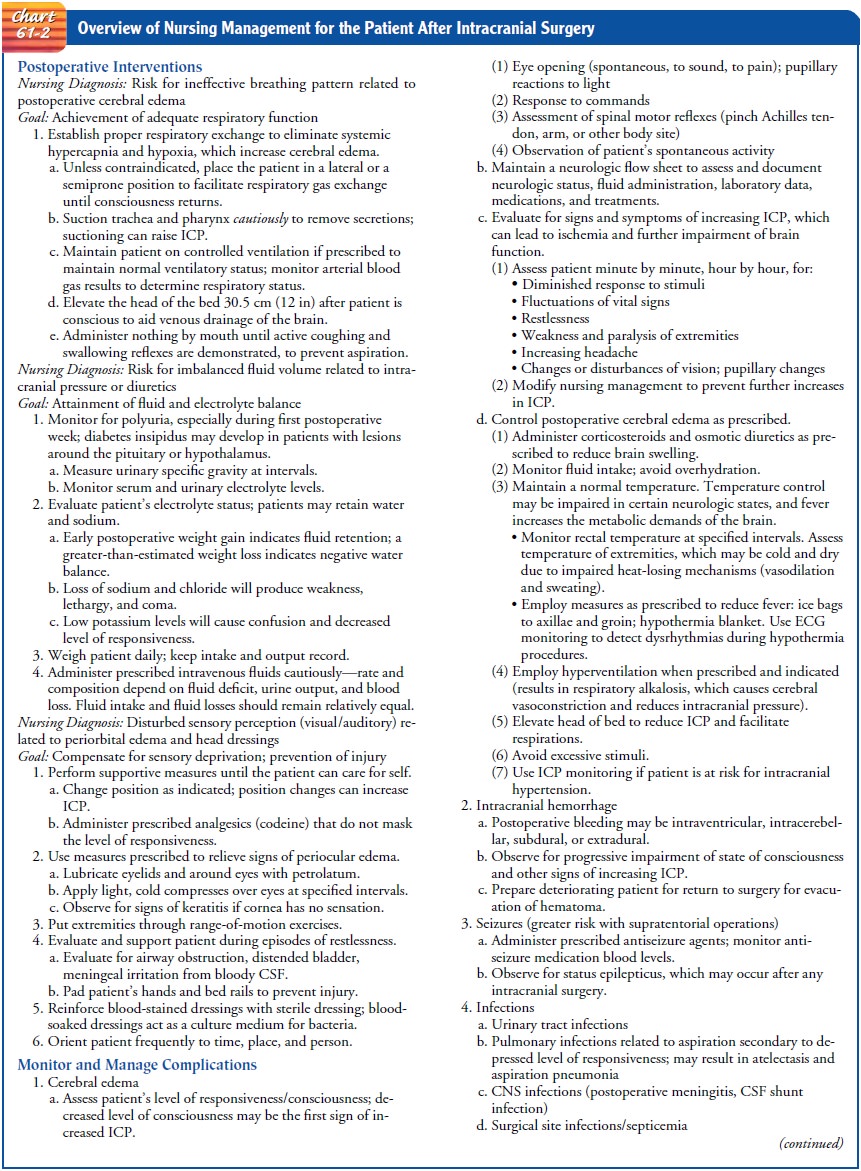
The
initial pattern of the seizures indicates the region of the brain in which the
seizure originates (see Chart 61-2). In simple partial seizures, only a finger
or hand may shake, or the mouth may jerk uncontrollably. The person may talk
unintelligibly, may be dizzy, and may experience unusual or unpleasant sights,
sounds, odors, or tastes, but without loss of consciousness (Greenberg, 2001;
Hickey, 2003).
In
complex partial seizures, the person either remains mo-tionless or moves automatically
but inappropriately for time and place, or may experience excessive emotions of
fear, anger, ela-tion, or irritability. Whatever the manifestations, the person
does not remember the episode when it is over.
Generalized
seizures, previously referred to as grand mal seizures, involve both
hemispheres of the brain, causing both sides of the body to react (Greenberg,
2001; Hickey, 2003). There may be intense rigidity of the entire body followed
by alternating muscle relaxation and contraction (generalized tonic–clonic
contrac-tion). The simultaneous contractions of the diaphragm and chest muscles
may produce a characteristic epileptic cry. The tongue is often chewed, and the
patient is incontinent of urine and stool. After 1 or 2 minutes, the convulsive
movements begin to subside; the patient relaxes and lies in deep coma,
breathing noisily. The respirations at this point are chiefly abdominal. In the
postictal state (after the seizure), the patient is often confused and hard to
arouse and may sleep for hours. Many patients complain of headache, sore
muscles, fatigue, and depression (Buelow, 2001).
Assessment and Diagnostic Findings
The
diagnostic assessment is aimed at determining the type of seizures, their
frequency and severity, and the factors that pre-cipitate them (Schachter,
2001). A developmental history istaken, including events of pregnancy and
childbirth, to seek evi-dence of preexisting injury. The patient is also
questioned about illnesses or head injuries that may have affected the brain. In
ad-dition to physical and neurologic evaluations, diagnostic exami-nations
include biochemical, hematologic, and serologic studies. MRI is used to detect
lesions in the brain, focal abnormalities, cerebrovascular abnormalities, and
cerebral degenerative changes (Schachter, 2001).
The electroencephalogram (EEG) furnishes diagnostic
evi-dence in a substantial proportion of patients with epilepsy and aids in
classifying the type of seizure (Schachter, 2001). Abnor-malities in the EEG
usually continue between seizures or, if not apparent, may be elicited by
hyperventilation or during sleep. Microelectrodes can be inserted deep in the
brain to probe the action of single brain cells. Some people with seizures have
nor-mal EEGs, whereas others who have never had seizures have ab-normal EEGs.
Telemetry and computerized equipment are used to monitor electrical brain
activity while patients pursue their normal activities and to store the
readings on computer tapes for analysis. Video recording of seizures taken simultaneously
with EEG telemetry is useful in determining the type of seizure as well as its
duration and magnitude. This type of intensive monitoring is changing the
treatment of severe epilepsy.
Single
photon emission computed tomography (SPECT) is an additional tool sometimes
used in the diagnostic workup. It is useful for identifying the epileptogenic
zone so that the area in the brain giving rise to seizures can be removed
surgically (Huntington, 1999).
Women With Epilepsy
More
than 1 million American women have epilepsy, and they face particular needs
associated with the syndrome (Schachter, Krishnamurthy & Cantrell, 2000).
Women with epilepsy often note an increase in seizure frequency during menses;
this has been linked to the increase in sex hormones that alter the
excitability of neurons in the cerebral cortex. Women of childbearing age
re-quire special care and guidance before, during, and after preg-nancy. Many
women note a change in the pattern of seizure activity during pregnancy. Fetal
malformation has been linked to the use of multiple antiseizure medications
(Karch, 2002). The effectiveness of contraceptives is decreased by antiseizure
med-ications. Therefore, patients should be encouraged to discuss family
planning with their primary health care provider and to obtain preconception
counseling if they are considering child-bearing (Liporace, 1997).
Because
of bone loss associated with the long-term use of anti-seizure medications,
patients receiving antiseizure agents should be assessed for low bone mass and
osteoporosis. They should be instructed about other strategies to reduce their
risks for osteoporosis.
Gerontologic Considerations
Elderly people have a high incidence of new-onset
epilepsy (Schachter, 2001). Increased incidence is associated with stroke, head
injury, dementia, infection, alcoholism, and aging. Treat-ment depends on the
underlying cause. Because many elderly people have chronic health problems,
they may be taking other medications that can interact with medications
prescribed for seizure control. In addition, the absorption, distribution,
metab-olism, and excretion of medications are altered in the elderly as a
result of age-related changes in renal and liver function. Therefore, the
elderly must be monitored closely for adverse and toxic effects of antiseizure
medications and for osteoporosis. The cost of antiseizure medications can lead
to poor adherence to the pre-scribed regimen in elderly patients on fixed
incomes.
Prevention
Society-wide efforts are the key to the prevention
of epilepsy. The risk for congenital fetal anomaly is two to three times higher
in mothers with epilepsy. The effects of maternal seizures, antiseizure
medications, and genetic predisposition are all mechanisms that contribute to
possible malformation. Because the unborn infants of mothers who take certain
antiseizure medications for epilepsy are at risk, these women need careful
monitoring, including blood studies to detect the level of antiseizure
medications taken through-out pregnancy (Karch, 2002). High-risk mothers
(teenagers, women with histories of difficult deliveries, drug use, patients
with diabetes or hypertension) should be identified and moni-tored closely
during pregnancy because damage to the fetus during pregnancy and delivery may
increase the risk for epilepsy. All of these issues need further study
(Schachter, Krishnamurthy & Cantrell, 2000).
Head
injury is one of the main causes of epilepsy that can be prevented.
Medical Management
The
management of epilepsy is individualized to meet the needs of each patient and
not just to manage and prevent seizures. Man-agement differs from patient to
patient because some forms of epilepsy arise from brain damage and others are
due to altered brain chemistry.
PHARMACOLOGIC THERAPY
Many
medications are available to control seizures, although the mechanisms of their
actions are still unknown (Karch, 2002). The objective is to achieve seizure
control with minimal side effects. Medication therapy controls rather than
cures seizures. Medications are selected on the basis of the type of seizure
being treated and the effectiveness and safety of the medications (Shafer,
1999a, 1999b; Winkelman, 1999). If properly prescribed and taken, medications
control seizures in 50% to 60% of patients with recurring seizures and provide
partial control in another 15% to 35%. The condition is not improved by any
available medication in 20% and 35% of patients with generalized and partial
epilepsy, respectively (Devinsky, 1999).
Treatment is usually started with a single medication.
The starting dose and the rate at which the dosage is increased depend on the
occurrence of side effects. The medication levels in the blood are monitored
because the rate of drug absorption varies among patients. Changing to another
medication may be neces-sary if seizure control is not achieved or if toxicity
makes it impossible to increase the dosage. The medication may need to be
adjusted because of concurrent illness, weight changes, or in-creases in
stress. Sudden withdrawal of these medications can cause seizures to occur with
greater frequency or can precipitate the development of status epilepticus
(Greenberg, 2001).
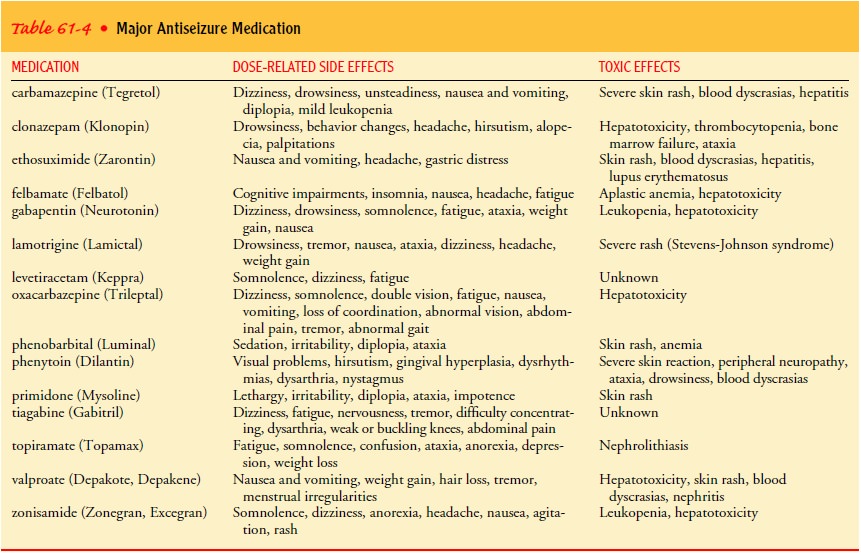
Side effects of antiseizure agents may be divided
into three groups: (1) idiosyncratic or allergic disorders, which present
pri-marily as skin reactions; (2) acute toxicity, which may occur whenthe
medication is initially prescribed; or (3) chronic toxicity, which occurs late
in the course of therapy.
The manifestations of drug toxicity are variable,
and any organ system may be involved. Gingival hyperplasia (swollen and tender
gums) can be associated with long-term use of phenyt-oin (Dilantin), for
example (Karch, 2002). Periodic physical and dental examinations and laboratory
tests are performed for pa-tients receiving medications known to have
hematopoietic, gen-itourinary, or hepatic effects. Table 61-4 lists the
medications in current use.
SURGICAL MANAGEMENT
Surgery is indicated for patients whose epilepsy
results from in-tracranial tumors, abscess, cysts, or vascular anomalies. Some
pa-tients have intractable seizure disorders that do not respond to medication.
There may be a focal atrophic process secondary to trauma, inflammation,
stroke, or anoxia. If the seizures originate in a reasonably well-circumscribed
area of the brain that can be excised without producing significant neurologic
deficits, the re-moval of the area generating the seizures may produce
long-term control and improvement (Wiebe, Blume, Girvin et al., 2001).
This type of neurosurgery has been aided by several
advances, including microsurgical techniques, depth EEGs, improved
illu-mination and hemostasis, and the introduction of neurolept-analgesic
agents (droperidol and fentanyl). These techniques, combined with use of local
anesthetic agents, enable the neuro-surgeon to perform surgery on an alert and
cooperative patient. Using special testing devices, electrocortical mapping,
and the pa-tient’s response to stimulation, the boundaries of the
epilepto-genic focus are determined (Huntington, 1999). Any abnormal
epileptogenic focus (ie, abnormal area of the brain) is then re-moved (Wiebe et
al., 2001).
As an adjunct to medication and surgery in
adolescents and adults with partial seizures, a generator may be implanted
under the clavicle. The device is connected to the vagus nerve in the cervical
area, where it delivers electrical signals to the brain to control and reduce
seizure activity (Kennedy & Schallert, 2001). An external programming
system is used by the physician to change stimulator settings. Patients can
turn the stimulator on and off with a magnet.
Related Topics