Chapter: Essential Anesthesia From Science to Practice : Applied physiology and pharmacology : A brief pharmacology related to anesthesia
The opioids
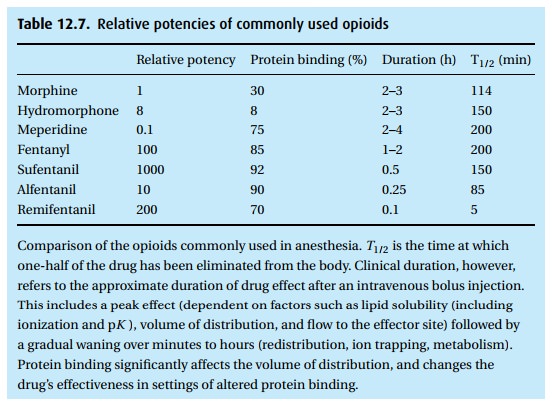
The opioids (Table 12.7)
Today,
narcotics play a major role in general anesthesia. Their advantage lies in
their potent ability to abolish pain without depressing the heart. Their
principle
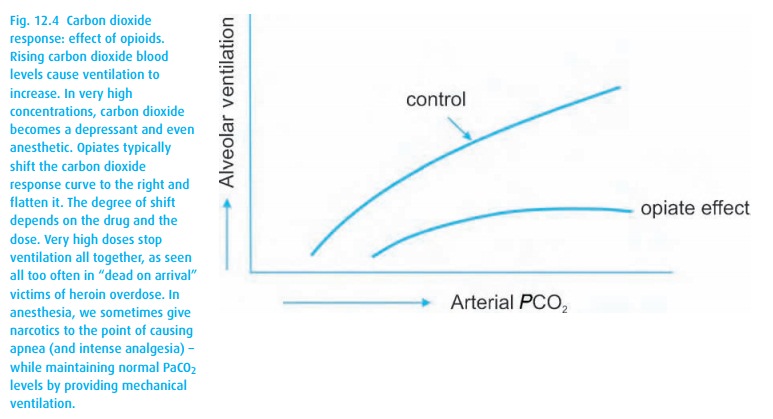
This side effect can be tol-erated if we are prepared to ventilate the
patient’s lungs, as we do routinely when patients receive neuromuscular
blocking drugs and thus require mechanical ven-tilation. Unchecked respiratory
depression and elevation of arterial carbon diox-ide can reduce resistance in
the arterial bed of the cerebral circulation, leading to increased intracranial
pressure. Chemoreceptor depression by opioids reduces the respiratory response
to hypoxemia; however, the administration of oxygen to a hypoxemic patient may
further depress ventilation, demonstrating that chemo-receptor activity still
contributes to the respiratory drive.
At this
time in anesthesia, we have no useful opioid that would spare the µ-2 receptors
responsible for respiratory depression, while exerting a full effect on the
receptors apparently involved in analgesia (µ-1, δ-1, δ-2 and κ-3 for
supraspinal analgesia, and µ-2, δ-2 and κ-1 for spinal analgesia). As mentioned
in the brief his-torical piece, to be eaten alive by a lion may not be painful,
presumably because the endogenous opioid polypeptides (the enkephalins,
endorphins, dynorphins and neoendorphins) kick in – evidently without causing
fatal respiratory depres-sion but presumably allowing for a gasp. We tend not
to rely on this physio-logic response to gourmand lions, even with the most
fearsome of surgeons at work.
Opioids
exhibit many side effects other than respiratory depression. Interesting to
anesthesia are the depressant effects on the autonomic nervous system with a
decrease in sympathetic tone and a preponderance of vagal activity, leading to
bradycardia and a reduction in blood pressure. The observed hypotension after
large doses of opioids gives evidence of venous pooling (exaggerated in
patients with a reduced blood volume) rather than a direct depressant effect on
the heart. Meperidine, having vagolytic effects, behaves somewhat differently.
During a
cholecystectomy, we need to be aware that opioids can increase the tone of the
sphincter of Oddi, thereby increasing pressure in the biliary system and interfering
with a surgeon’s attempt to perform a cholangiogram.
Opioids
have numerous side effects in addition to respiratory depression. These range
from miosis (the infamous pin-point pupils – again meperidine is the
excep-tion), itching, constipation and nausea, to changes in mood (either
euphoria or dysphoria, depending on the setting and the patient). Some of these
effects have their origin locally (constipation), others centrally
(chemoreceptor stimulation triggering nausea).
By now
the opioids have amassed quite a retinue of narcotic compounds, some of which
appear to have unrelated chemical footprints. While heroin, codeine, and many
relatives show their kinship with morphine, others are classified as
piperidines and phenylpiperidines, comprising meperidine and the different
fen-tanyl drugs.
Morphine
Morphine
(Fig. 12.5) has a long tradition as an
analgesic for wound pain with a typical i.m. dose of 10 mg for a 70 kg patient.
Despite its propensity to stimulate his-tamine release, we make extensive use of
i.v. morphine for management of acute pain, as an intra-operative analgesic and
adjunct to general anesthesia, and post-operatively as the most common drug for
patient-controlled analgesia (PCA). We also commonly administer morphine
neuraxially (epidural or subarachnoid) to obtain 18–24 hours of post-surgical
analgesia, though delayed respiratory depres-sion remains a concern. One of its
metabolites, morphine-6-glucuronide, retains much of morphine’s activity and
has been implicated in prolonged respiratory depression observed in patients
with renal failure.
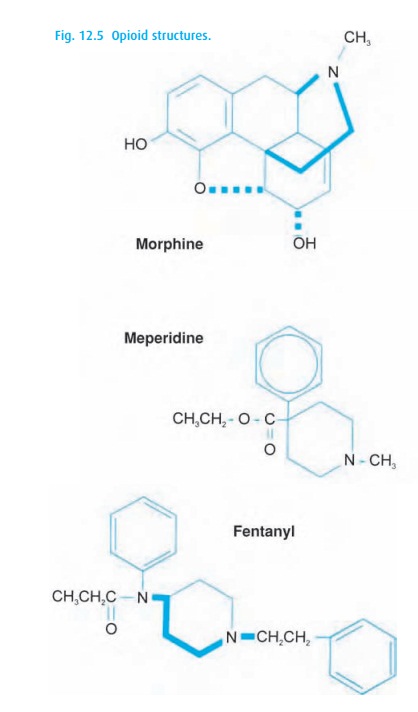
Meperidine (pethidine, Demerol®, Dolantin®, Pethadol®)
Another
synthetic opioid, meperidine, deserves to be mentioned, though in anes-thesia
we use it less today than before the arrival of its chemical grandchildren, the
fentanyls. Meperidine (Fig. 12.5), with 1/10
the potency and shorter dura-tion of action than morphine, occupies a unique
spot among opioids in its anti-muscarinic activity. Patients receiving
meperidine do not develop the “pin-point pupils” we expect with other opioids;
they may also become tachycardic and complain of a dry mouth. The drug can be
associated with nausea and vomiting as well. Most importantly, it should not be
given to patients taking monoamine oxidase inhibitors because severe
respiratory depression, excitation, and even convulsions can be the consequence
(serotonin syndrome). Meperidine’s main metabolite, normeperidine, lasts for
days (T1/2 elimination = 15–40 h). Particularly in the setting of impaired renal function, the
accumulation of normeperidine can cause myoclonus and seizures.
Fentanyls
Fentanyl (Sublimaze®) (Fig. 12.5), with a potency 100 times that of morphine, has even more potent offspring. The growing list includes 3-methyl fentanyl, lofentanyl, and etorphin being several thousand-fold as potent as morphine. None have made it into the operating room. Nor are they needed as potency in the clinical setting means relatively little as long as the desired effect can be reached by adjusting the dose, and as long as that dose can be readily delivered. Clinical doses of the fentanyls are all in the microgram/kg range, thus posing no difficulty to intravenous administration.
The
differences among the fentanyls reside primarily in the duration of action,
since, in general, the respiratory depressant effect runs parallel with the
analgesic effectiveness. There are small differences in the onset of action
after an intra-venous bolus, with fentanyl and sufentanil (Sufenta®) taking
about 6 minutes for the peak effect to set in while alfentanil (Alfenta®) and
remifentanil (Ultiva®) reach their peaks in about a minute. Remifentanil, an
ester, deserves special men-tion as the only narcotic that falls prey to
non-specific plasma esterases that hydrolyze the drug, thus rapidly curtailing
its effect. The other opioids have to rely on liver blood flow and hepatic
biotransformation. A comparison of each of the commonly used opioids may be of
help (Table 12.7).
Finally,
let us mention that narcotic addiction has not spared anesthesia and nursing
personnel. Easy access to narcotics has been blamed for the higher frequency of
addiction among anesthesia personnel than other health care workers.
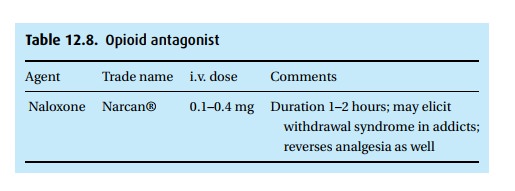
Opioid receptor antagonism: naloxone (Narcan®)
Opioids
are antagonized by naloxone, chemically related to morphine and com-peting for
receptor sites occupied by the agonists (See Table 12.8).
In the adult, we usually start with 40–100 mcg naloxone intravenously,
expecting to see a response within a minute. The half-life of the drug is
around 40 minutes. Thus, patients who had been depressed by the longer acting
drugs, such as morphine, must be observed for at least an hour in order not to
miss recurring respiratory depression. In addicted patients under the influence
of and tolerant to large doses of a narcotic analgesic, a larger dose of
naloxone can trigger a stormy withdrawal reaction, as can administration of
some of the mixed agonist-antagonist drugs, among them butorphanol (Stadol®)
and nalbuphine (Nubain®). These latter agents have a ceiling effect on
respiratory depression, a property considered vital in obstetrics where they
are commonly used – never mind that the patient’s pain is not much relieved by
these agents!
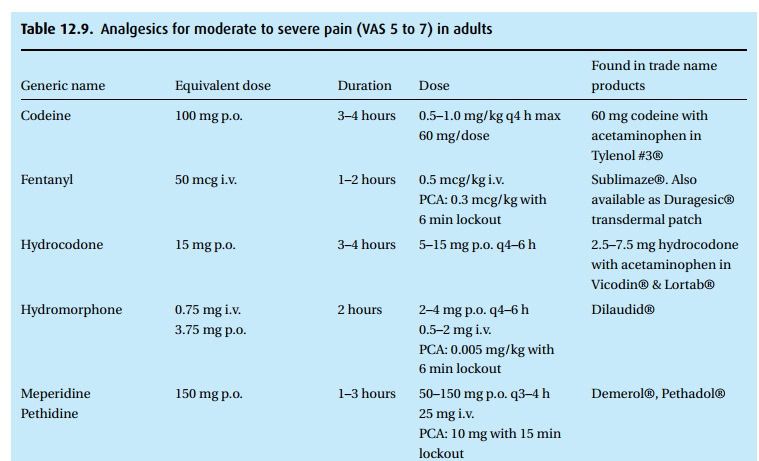
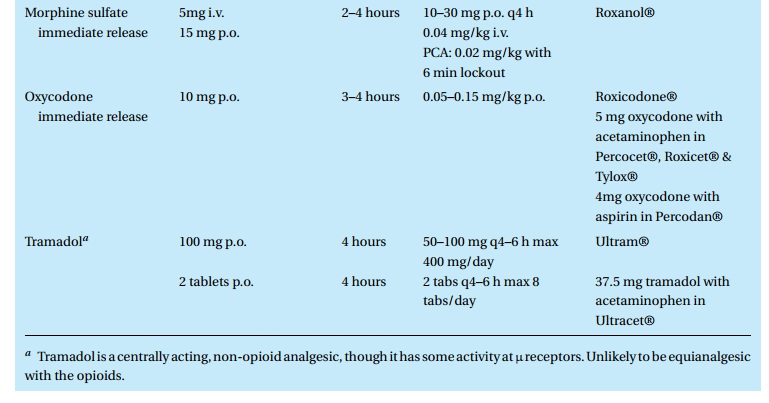
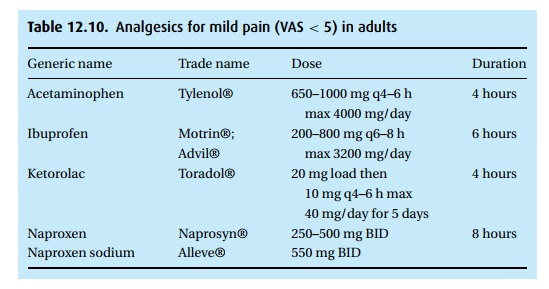
Clinical perspectives on the use of analgesics
In the
chapter on Post-operative care, you will find a discussion of how to assess the
severity of pain. Many different drugs find use in the treatment of pain. The
following tables are not intended to guide therapy, but are presented here for
the sake of orientation. We do not offer a discussion of these drugs and urge
the reader to consult pharmacologic texts and the information offered by the
manufacturers. For moderate to severe pain (VAS 5 to 7), you may see one of the
drugs in Table 12.9prescribed. For mild pain
we often use one of the common oral, non-narcotic analgesics that are available
over the counter (Table 12.10).
Related Topics