Chapter: Basic & Clinical Pharmacology : Pancreatic Hormones & Antidiabetic Drugs
The Endocrine Pancreas
THE ENDOCRINE PANCREAS
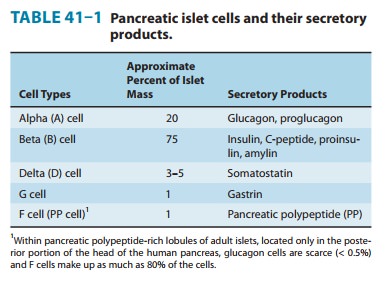
The endocrine pancreas
in the adult human consists of approxi-mately 1 million islets of Langerhans
interspersed throughout the pancreatic gland. Within the islets, at least four
hormone-producing cells are present (Table 41–1). Their hormone products
include insulin, the storage and
anabolic hormone of the body; islet
amy-loid polypeptide (IAPP, or
amylin), which modulates appetite,gastric emptying, and glucagon and
insulin secretion; glucagon, the
hyperglycemic factor that mobilizes glycogen stores; somatostatin, a universal inhibitor of secretory cells; gastrin, which stimulates gastric acid
secretion; and pancreatic peptide, a
small protein that facilitates digestive processes by a mechanism not yet
clarified.
Diabetes mellitus is
defined as an elevated blood glucose asso-ciated with absent or inadequate
pancreatic insulin secretion, with or without concurrent impairment of insulin
action. The disease states underlying the diagnosis of diabetes mellitus are
now classified into four categories: type 1, insulin-dependent diabetes; type 2,non–insulin-dependent diabetes; type 3, other; and type 4,
gesta-tional diabetes mellitus (Expert Committee, 2003).
Type 1 Diabetes Mellitus
The hallmark of type 1
diabetes is selective beta cell (B cell) destruction and severe or absolute
insulin deficiency. Type 1 diabetes is further subdivided into immune and
idiopathic causes. The immune form is the most common form of type 1 diabetes.
Although most patients are younger than 30 years of age at the time of
diagnosis, the onset can occur at any age. Type 1 diabetes is found in all
ethnic groups, but the highest incidence is in people from northern Europe and
from Sardinia. Susceptibility appears to involve a multifactorial genetic
linkage, but only 10–15% of patients have a positive family history.
For persons with type
1 diabetes, insulin replacement therapy is necessary to sustain life.
Pharmacologic insulin is administered by injection into the subcutaneous tissue
using a manual injection device or an insulin pump that continuously infuses
insulin under
Interruption
of the insulin replacement therapy can be life-threatening and can result in diabetic ketoacidosis or death.
Diabetic ketoacidosis is caused by insufficient or absent insulin and results
from excess release of fatty acids and subsequent formation of toxic levels of
ketoacids.
Type 2 Diabetes Mellitus
Type 2 diabetes is
characterized by tissue resistance to the action of insulin combined with a relative deficiency in insulin
secretion. A given individual may have more resistance or more beta-cell
deficiency, and the abnormalities may be mild or severe. Although insulin is
produced by the beta cells in these patients, it is inade-quate to overcome the
resistance, and the blood glucose rises. The impaired insulin action also
affects fat metabolism, resulting in increased free fatty acid flux and
triglyceride levels and reciprocally low levels of high-density lipoprotein
(HDL).
Individuals
with type 2 diabetes may not require insulin to sur-vive, but 30% or more will
benefit from insulin therapy to control blood glucose. It is likely that 10–20%
of individuals in whom type 2 diabetes was initially diagnosed actually have
both type 1 and type 2 or a slowly progressing type 1 called latent autoimmune
diabetes of adults (LADA), and they ultimately require full insulin
replace-ment. Although persons with type 2 diabetes ordinarily do not develop
ketosis, ketoacidosis may occur as the result of stress such as infection or
the use of medication that enhances resistance, eg, cor-ticosteroids.
Dehydration in individuals with untreated or poorly controlled type 2 diabetes
can lead to a life-threatening condition called nonketotic hyperosmolar coma. In this condition, the blood glucose
may rise to 6–20 times the normal range and an altered mental state develops or
the person loses consciousness. Urgent medical care and rehydration are
required.
Type 3 Diabetes Mellitus
The
type 3 designation refers to multiple other
specific causes of an elevated blood glucose: pancreatectomy, pancreatitis,
nonpancreatic diseases, drug therapy, etc. For a detailed list the reader is
referred to the reference Expert Committee, 2003.
Type 4 Diabetes Mellitus
Gestational
diabetes (GDM) is defined as any abnormality in glucose levels noted for the
first time during pregnancy. Gestational diabetes is diagnosed in approximately
7% of all pregnancies in the USA. During pregnancy, the placenta and placental
hormones create an insulin resistance that is most pronounced in the last
trimester. Risk assessment for diabetes is suggested starting at the first
prenatal visit. High-risk women should be screened immedi-ately. Screening may
be deferred in lower-risk women until the 24th to 28th week of gestation.
Related Topics