Chapter: Basic & Clinical Pharmacology : Pancreatic Hormones & Antidiabetic Drugs
Alpha-Glucosidase Inhibitors
ALPHA-GLUCOSIDASE INHIBITORS
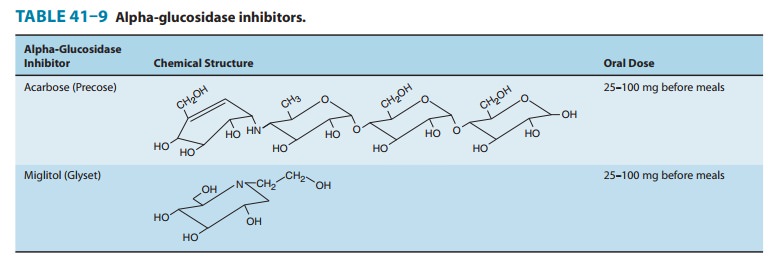
Acarbose and miglitol are
competitive inhibitors of the intestinalα-glucosidases and reduce postmeal glucose
excursions by delay-ing the digestion and absorption of starch and
disaccharides (Table 41–9). Only monosaccharides, such as glucose and
fruc-tose, can be transported out of the intestinal lumen and into the bloodstream.
Complex starches, oligosaccharides, and disaccha-rides must be broken down into
individual monosaccharides before being absorbed in the duodenum and upper
jejunum. This digestion is facilitated by enteric enzymes, including pancreatic
α-amylase
and α-glucosidases
that are attached to the brush bor-der of the intestinal cells. Miglitol
differs structurally from acar-bose and is six times more potent in inhibiting
sucrase. Although the binding affinity of the two compounds differs, acarbose
and miglitol both target the α-glucosidases: sucrase, maltase,
glu-coamylase, and dextranase. Miglitol alone has effects on isomaltase and on β-glucosidases, which
split β-linked
sugars such as lactose. Acarbose alone has a small effect on α-amylase. The
consequence of enzyme inhibition is to minimize upper intestinal digestion and
defer digestion (and thus absorption) of the ingested starch and disaccharides
to the distal small intestine, thereby lowering post-meal glycemic excursions
as much as 45–60 mg/dL and creating an insulin-sparing effect.
Monotherapy with these
drugs is associated with a modest drop (0.5–1%) in glycohemoglobin levels and a
20–25 mg/dL fall in fasting glucose levels. They are FDA-approved for persons
with type 2 diabetes as monotherapy and in combination with sulfo-nylureas, in
which the glycemic effect is additive. Both acarbose and miglitol are taken in
doses of 25–100 mg just before ingesting the first portion of each meal;
therapy should be initiated with the lowest dose and slowly titrated upward,
and a similar amount of starch and disaccharides should be ingested at each
meal.
Prominent adverse
effects include flatulence, diarrhea, and abdominal pain and result from the
appearance of undigested carbohydrate in the colon that is then fermented into
short-chain fatty acids, releasing gas. These adverse effects tend to diminish
with ongoing use because chronic exposure to carbohydrate induces the
expression of α-glucosidase
in the jejunum and ileum, increas-ing distal small intestine glucose absorption
and minimizing the passage of carbohydrate into the colon. Although not a
problem with monotherapy or combination therapy with a biguanide, hypoglycemia
may occur with concurrent sulfonylurea treatment. Hypoglycemia should be
treated with glucose (dextrose) and not sucrose, whose breakdown may be
blocked. These drugs are con-traindicated in patients with inflammatory bowel
disease or any intestinal condition that could be worsened by gas and
distention. Because both miglitol and acarbose are excreted by the kidneys,
these medications should not be prescribed in individuals with renal
impairment. Acarbose has been associated with reversible hepatic enzyme
elevation and should be used with caution in the presence of hepatic disease.
The STOP-NIDDM trial demonstrated that α-glucosidase therapy in prediabetic persons successfully prevented a significant number of new cases of type 2 diabetes and helped restore beta-cell function, in addition to reducing cardiovascular disease and hypertension. Intervention with acarbose also reduced cardiovas-cular events in persons with diabetes. Diabetes and cardiovascular disease prevention may become a further indication for this class of medications.
Alpha-glucosidase
inhibitors are infrequently prescribed in the United States because of their
prominent gastrointestinal adverse effects and relatively minor
glucose-lowering benefit.
Related Topics