Chapter: Basic & Clinical Pharmacology : Pancreatic Hormones & Antidiabetic Drugs
Insulin Delivery Systems
Insulin Delivery Systems
A. Standard Delivery
The
standard mode of insulin therapy is subcutaneous injection using conventional
disposable needles and syringes.
B. Portable Pen Injectors
To facilitate multiple
subcutaneous injections of insulin, particu-larly during intensive insulin
therapy, portable pen-sized injectors have been developed. These contain
cartridges of insulin and replaceable needles.
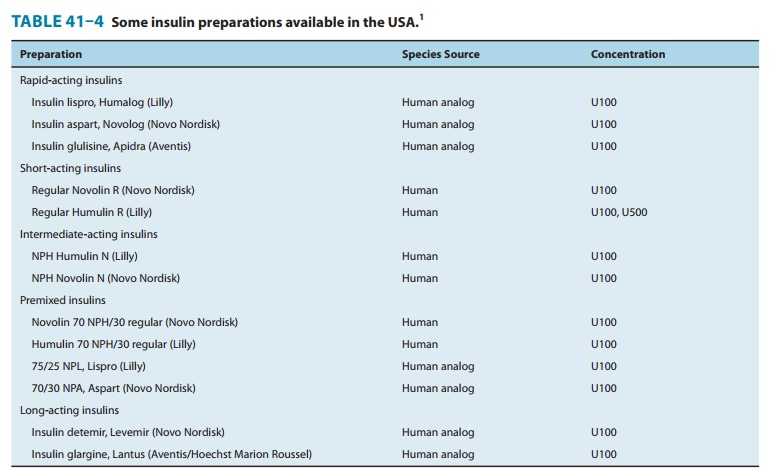
Disposable insulin
pens are also available for selected formula-tions. These are regular insulin,
insulin lispro, insulin aspart, insu-lin glulisine, insulin glargine, insulin
detemir, and several mixtures of NPH with regular, lispro, or aspart insulin
(Table 41–4). They have been well accepted by patients because they eliminate
the need to carry syringes and bottles of insulin to the workplace and while
traveling.
C. Continuous Subcutaneous Insulin Infusion Devices (CSII, Insulin Pumps)
Continuous
subcutaneous insulin infusion devices are external open-loop pumps for insulin
delivery. The devices have a user-programmable pump that delivers
individualized basal and bolus insulin replacement doses based on blood glucose
self-monitoring results.
Normally, the 24-hour
background basal rates are prepro-grammed and relatively constant from day to
day, although tem-porarily altered rates can be superimposed to adjust for a
short-term change in requirement. For example, the basal delivery rate might
need to be decreased for several hours because of the increased insulin
sensitivity associated with strenuous activity.
Boluses
are used to correct high blood glucose levels and to cover mealtime insulin
requirements based on the carbohydrate content of the food and concurrent
activity. Bolus amounts are either dynamically programmed or use preprogrammed
algo-rithms. When the boluses are dynamically programmed, the user calculates
the dose based on the amount of carbohydrate con-sumed and the current blood
glucose level. Alternatively, the meal or snack dose algorithm (grams of
carbohydrate covered by a unit of insulin) and insulin sensitivity or blood
glucose correc-tion factor (fall in blood glucose level in response to a unit
of insulin) can be preprogrammed into the pump. If the user enters the
carbohydrate content of the food and current blood glucose value, the insulin
pump will calculate the most appropriate dose of insulin. Advanced insulin
pumps also have an “insulin on board” feature that adjusts a high blood glucose
correction dose to correct for residual activity of previous bolus doses.
The traditional
pump—which contains an insulin reservoir, the program chip, the keypad, and the
display screen—is about the size of a pager. It is usually placed on a belt or
in a pocket, and the insulin is infused through thin plastic tubing that is
connected to the subcutaneously inserted infusion set. The abdomen is the
favored site for the infusion set, although flanks and thighs are also used.
The insulin reservoir, tubing, and infusion set need to be changed using
sterile techniques every 2 or 3 days. Currently, only one pump does not require
tubing. In this model, the pump is attached directly to the infusion set.
Programming is done through a hand-held unit that communicates wirelessly with
the pump. CSII delivery is regarded as the most physiologic method of insu-lin
replacement.
Use of these
continuous infusion devices is encouraged for people who are unable to obtain
target control while on multiple injection regimens and in circumstances in
which excellent glyce-mic control is desired, such as during pregnancy. Optimal
use of these devices requires responsible involvement and commitment by the
patient. Insulin aspart, lispro, and glulisine all are specifi-cally approved
for pump use and are preferred pump insulins because their favorable
pharmacokinetic attributes allow glycemic control without increasing the risk
of hypoglycemia.
Related Topics