Chapter: Medicine Study Notes : Respiratory
Restrictive/Interstitial Pulmonary Disease
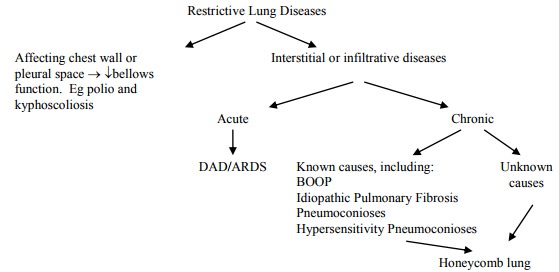
Restrictive/Interstitial Pulmonary Disease
·
= Reduced expansion of the lung
parenchyma
·
British and Americans give them
different names
·
Over 150 different disease
processes primarily affecting alveoli epithelium, interstitium and capillary
endothelium, not airways
·
Leads to ¯expansion
of lung parenchyma, ¯total lung capacity, ¯lung compliance
·
Other causes:
o Secondary to drugs (eg amiodarone)
o Secondary to radiotherapy
o In some connective tissue diseases (eg Ankylosing Spondylitis)
Acute Interstitial Lung Disease
Adult Respiratory Distress
Syndrome (ARDS)
·
= Diffuse Alveolar Damage (DAD)
·
= Shock Lung
·
Clinical: rapid onset of
life-threatening respiratory insufficiency, cyanosis and hypoxaemia refractory
to O2 therapy
·
Diagnostic criteria: acute onset,
fluid on CXR, capillary wedge pressure < 19 (Þ not LH
failure), hypoxia
·
Aetiology – types of injury:
o Aspiration: gastric contents or drowning
o Inhalation of fumes or toxic aerosols, smoke, chlorine, oxygen toxicity
o Circulating toxins: bacterial endotoxins
o Other: DIC, high altitude, trauma, radiation therapy, chemotherapy
·
Pathogenesis:
o Results from leakage from capillaries to alveoli spaces: non-cardiogenic
pulmonary oedema
o Leads to a non-compliant lung: smaller tidal volume, poor gas exchange, risk of
lung rupture when ventilating
o Prototypical injury is oxygen toxicity: hyperoxia damage alveolar
macrophages (AM) ® release O2 radicals ® injure lung tissue; AM release
cytokines ® attract neutrophils, stimulate intravascular adherence, and release
further O2 radicals. Vicious circle of damage, especially to septum
o Other possible initiating mechanisms (alone or in combination):
activation of complement cascade, neutrophil aggregation, activation of
coagulation ® fibrin deposition, etc
·
Macroscopic appearance: Affects
WHOLE lung (if only one lobe affected ?pneumonia). Heavy lungs due to fluid
accumulation (interstitial and later alveolar)
·
Microscopic appearance:
o Early change: interstitial oedema, few cell infiltrates
o Acute exudative stage: microvascular injury ®
breakdown of basement membrane ® leakage of plasma proteins into alveoli. Sloughing of injured type 1
pneumocytes. Cell debris + exudate form hyaline membrane. Inflammatory cells in
interstitium. No neutrophils in alveoli (key differential from pneumonia)
o Proliferative stage: Type II pneumocytes proliferate to cover alveolar
surface. Fibroblasts lay down collagen in interstitium and alveolar spaces ®
interstitial and intra-alveolar fibrosis
·
Prognosis: 50% mortality.
Surviving patients may have mild to extensive diffuse interstitial pulmonary
fibrosis
Acute Interstitial Pneumonia (AIP)
·
= Hamman-Rich Disease
·
Rapidly progressive interstitial
pneumonitis that resembles the organising stage of DAD (?may be a variant)
·
Affects young adults, presenting
with flu-like syndrome and bilateral infiltrates. Most die of respiratory
failure within two months
Chronic Infiltrative (Restrictive) Lung Disease
·
Common clinical and radiologic
features but diverse aetiology and pathology
·
Clinical features:
o Cyanosis due to severe hypoxemia from ventilation-perfusion mismatch
o Clubbing of digits
o Late in disease: pulmonary hypertension due to destruction of alveolar
capillary bed
o Interstitial infiltrate and some exudate in small airspaces
·
Diseases leading to chronic
infiltrative lung disease:
o Idiopathic chronic interstitial pneumonias: 13%
o Environmental lung disease: 25%
o Sarcoidosis: 20%
Types of Idiopathic Pulmonary Fibrosis (IPF)
·
Usual Interstitial Pneumonia
(UIP, US):
o = Cryptogenic Fibrosing Alveolitis (UK)
o Most common type of IPF
o Presents with gradual onset of dyspnoea and cough (usually dry)
o Non-uniform slowly progressive disease starting in middle age. Die in
several years. No known treatment (don‟t respond to steroids). Airflow and
blood flow disrupted
o Macroscopic appearance: when advanced lung is small and firm with a
honeycomb appearance on cut section
o Microscopic appearance: ranges from normal to fibrotic alveolar walls,
with marked variation in the degree of fibrosis from field to field (cf other
IPFs which are uniform). Capillary bed slowly destroyed ®
pulmonary hypertension and cor pulmonale. Inflammatory cells (lymphocytes +
macrophages + neutrophils) in interstitium and airspaces
·
Desquamative Interstitial
Pneumonia (DIP): more uniform than UIP, with no alternating areas of scarring
and normal lung. Filling of alveolar with alveolar macrophages (not desquamated
as originally thought). Is it an early stage of UIP? However, may respond to
steroids and have a better prognosis. X-ray shows bilateral lower lobe ground
glass infiltrates
·
Lymphocytic Interstitial
Pneumonia (LIP)
·
Granulomatous Interstitial
Pneumonia
Bronchiolitis Obliterans Organising Pneumonia (BOOP)
·
Obliterans Þ airways
sealed off
·
Organising Þ fibrosis
· Common response to lung injury from infections, inhaled toxins, drugs, etc
·
Major finding: plugs of loose
fibrous tissue filling bronchioles and alveoli. Variable chronic inflammatory
cell infiltrate is present
·
Patients improve gradually with
steroids (ie different from UIP)
Pneumoconioses
·
= Pulmonary diseases caused by
the inhalation of inorganic dust (usually stimulating fibrosis)
·
Asbestos:
o Occupational exposure to asbestos is linked to:
§ Localised fibrous plaques: dense fibrotic plaques on X-ray – generally
asymptomatic
§ Pleural effusions ® cough, SOB
§ Asbestosis: Parenchymal interstitial fibrosis. Progressive SOB on
exertion. ¯FVC, ¯FEV but FEV/FVC, ¯DL CO, restrictive pattern
§ Bronchogenic carcinoma (5 times risk, 14 times risk if smoker): most
common
§ Mesotheliomas (1000 times risk) but still rare.
§ Laryngeal and perhaps extrapulmonary neoplasms
o When asking about occupational exposure, need to go back a long time.
Will present in an older man. Ask them what they did when they left school and
go from there.
o Pathogenesis: depends on which type of asbestos. Serpentine crysotile
form (curly, flexible) is more common, less dangerous, cleared more easily from
bronchi and more soluble so don‟t persist in the alveoli. Amphibole type (straight,
stiff, brittle) rarer, more dangerous, go deeper, penetrate epithelial cells
and lodge in the interstitium
·
Coal Workers Pneumoconiosis
(CWP):
o Two forms:
§ Simple CWP: accumulation of dust laden macrophages with little pulmonary
dysfunction
§ Complicated CWP: progressive fibrosis induced by macrophages
o Macroscopic appearance: Anthracosis, coal nodules progressing to black
scars larger than 2 cm in complicated CWP
o Microscopic appearance: Coal laden macrophages, fibrous scarring
o Caplan‟s Syndrome: Rheumatoid arthritis with a pneumoconiosis ® nodular
pulmonary lesions
·
Silicosis:
o Exposure to crystalline silicon dioxide: sand blasting, rock mining,
foundry work
o Silica causes activation and release of inflammatory factors by
macrophages
o Morphology: discrete pale to black tiny nodules which coalesce into
fibrous scars
Hypersensitivity Pneumonia
·
= Extrinsic Allergic Alveolitis
· Sometimes grouped with Pneumoconioses ® Occupational Lung Disease
·
Immune resistance to protein
antigens ® acute or chronic attacks on re-exposure
·
Lots of causes: farmer‟s lung
(antigen is thermophilic actinomyces), pigeon breeder HSP, air-conditioner HSP
·
Morphology: chronic inflammatory
cells in the alveolar septi, septal fibrosis, obliterative bronchiolitis and
non-necrotising granuloma formation (diagnostic on biopsy)
Honey Comb Lung
·
End stage of many chronic
interstitial lung diseases
·
Morphology: small lungs with
nodular pleural surface due to interstitial fibrosis retracting the pleura.
Large air spaces cause honeycomb effect. Destruction of the capillary bed in
the lung ® pulmonary hypertension, RV hypertrophy, cor pulmonale ® death
Sarcoidosis
·
Multisystem disorder, most common
in the young and in females
·
Aetiology: ?antigenic stimulus ® cell
mediated (type 4) immune injury
·
Pathogenesis: poorly understood.
Deficient cell mediated immunity. Eg anergic to the TB skin test. Stimulated
B-cell population with resultant hyperglobulinaemia. ?Antigen ® T cells
inducing B cells. Monocytes recruited ® granuloma formation
·
Macroscopic appearance: Chest
X-ray shows bilateral hilar lymphadenopathy and/or diffuse interstitial
disease. Granulomas also found in spleen, liver, bone marrow, skin, eye and
salivary glands
·
Microscopic appearance:
non-caseating (non-necrotic) granulomas (unlike TB). Occur in all organs but
most commonly in all parts of the lungs. Tightly clustered epithelioid
histiocytes, multiple giant cells, and a few peripheral lymphocytes
·
Clinical course: Treat with steroids. 70% recover, 20% have some loss of function,
10% die
Related Topics