Chapter: Medicine Study Notes : Respiratory
Acute Interstitial Lung Disease
Restrictive/Interstitial Pulmonary Disease
· = Reduced expansion of the lung parenchyma
· British and Americans give them different names
· Over 150 different disease processes primarily affecting alveoli epithelium, interstitium and capillary endothelium, not airways
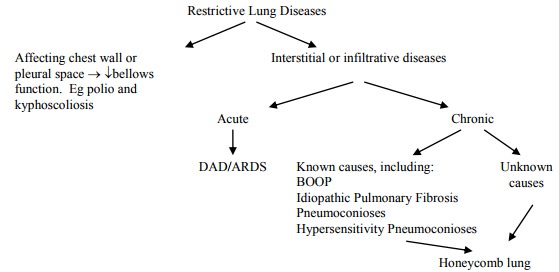
· Leads to ¯expansion of lung parenchyma, ¯total lung capacity, ¯lung compliance
· Other causes:
o Secondary to drugs (eg amiodarone)
o Secondary to radiotherapy
o In some connective tissue diseases (eg Ankylosing Spondylitis)
Acute Interstitial Lung Disease
Adult Respiratory Distress Syndrome (ARDS)
·
= Diffuse Alveolar Damage (DAD)
·
= Shock Lung
·
Clinical: rapid onset of
life-threatening respiratory insufficiency, cyanosis and hypoxaemia refractory
to O2 therapy
·
Diagnostic criteria: acute onset,
fluid on CXR, capillary wedge pressure < 19 (Þ not LH
failure), hypoxia
·
Aetiology – types of injury:
o Aspiration: gastric contents or drowning
o Inhalation of fumes or toxic aerosols, smoke, chlorine, oxygen toxicity
o Circulating toxins: bacterial endotoxins
o Other: DIC, high altitude, trauma, radiation therapy, chemotherapy
·
Pathogenesis:
o Results from leakage from capillaries to alveoli spaces: non-cardiogenic
pulmonary oedema
o Leads to a non-compliant lung: smaller tidal volume, poor gas exchange, risk of
lung rupture when ventilating
o Prototypical injury is oxygen toxicity: hyperoxia damage alveolar
macrophages (AM) ® release O2 radicals ® injure lung tissue; AM release
cytokines ® attract neutrophils, stimulate intravascular adherence, and release
further O2 radicals. Vicious circle of damage, especially to septum
o Other possible initiating mechanisms (alone or in combination):
activation of complement cascade, neutrophil aggregation, activation of
coagulation ® fibrin deposition, etc
·
Macroscopic appearance: Affects
WHOLE lung (if only one lobe affected ?pneumonia). Heavy lungs due to fluid
accumulation (interstitial and later alveolar)
·
Microscopic appearance:
o Early change: interstitial oedema, few cell infiltrates
o Acute exudative stage: microvascular injury ®
breakdown of basement membrane ® leakage of plasma proteins into alveoli. Sloughing of injured type 1
pneumocytes. Cell debris + exudate form hyaline membrane. Inflammatory cells in
interstitium. No neutrophils in alveoli (key differential from pneumonia)
o Proliferative stage: Type II pneumocytes proliferate to cover alveolar
surface. Fibroblasts lay down collagen in interstitium and alveolar spaces ®
interstitial and intra-alveolar fibrosis
·
Prognosis: 50% mortality.
Surviving patients may have mild to extensive diffuse interstitial pulmonary
fibrosis
Acute Interstitial Pneumonia (AIP)
·
= Hamman-Rich Disease
·
Rapidly progressive interstitial
pneumonitis that resembles the organising stage of DAD (?may be a variant)
·
Affects young adults, presenting
with flu-like syndrome and bilateral infiltrates. Most die of respiratory
failure within two months
Related Topics