Chapter: Medicine Study Notes : Respiratory
Neoplasia of the Respiratory Tract
Neoplasia of the Respiratory Tract
Cancer of the Nasal Cavity and Paranasal Sinuses
·
Inflammatory Polyp:
o Not a true tumour: overgrowth of stromal tissue – no malignant potential
o Common in adults, rare in children
o Associated with cystic fibrosis
· Sinonasal papilloma:
o Benign. Can become malignant. 3% become malignant after removal (poor
prognosis). 3% have malignancy in polyp (prognosis better)
o Usually in adult. Presents with
nasal obstruction and painless epistaxis
o ?Associated with HPV 6 & 11
·
Sinonasal Carcinoma:
o Occupational association: wood turners (adenocarcinoma) and nickel
mining
o Relatively rare (<1% of cancer deaths)
o 60% 5 year survival, surgical treatment
o Squamous cell most common (look for keratin whirls), also adenocarcinoma
o Stromal overgrowth = desmoplasia Þ sign of invasive cancer
·
Nasopharyngeal Carcinoma:
o Most common in SE Asia and N Africa, occurs in 15 – 25 and 60 – 69.
Presents with epistaxis or obstructed eustachian
o No occupational association
o Associated with EBV
o Biphasic tumour: Small cells superimposed on squamous cell carcinoma,
with lots of lymphocytes
o (don‟t confuse with lymphoma)
o Aggressive: early lymph node spread
o Treatment: radiotherapy +/- surgery
Tumours of the Larynx
·
Benign non-neoplastic neck lumps:
o Inflammatory:
§ Lymph nodes: anterior cervical for tonsillitis, jugular digastric for
tongue
§ Atypical Tb (especially kids)
§ Deep Neck abscesses: para-pharyngeal or retro-pharyngeal abscesses (can
track down into mediastinum)
o Thyroglossal cysts: cysts in embryological track from tongue to thyroid
(usually at level of hyoid)
o Branchial cysts: ?embryological.
Like enlarged anterior node.
Contain lots of cholesterol
o Pharyngeal pouch: Mucosa herniates out through triangle between the cricopharyngeus
and thyropharyngeal muscles under pressure from swallowing when upper
oesophageal sphincter doesn‟t relax properly. Catches food, becomes infected.
Treatment: surgery
·
Laryngeal Nodule:
o Due to trauma of vocal chords banging together ® oedema (early)
® scarring/granulation tissue (late)
o Only on anterior 1/3rd of vocal fold
o Completely benign
o Gravely voice
·
Laryngeal Papilloma:
o Like sinonasal papillomas
o Most commonly seen in children
o Associated with HPV 6, 11
o Tendency to recur: can become unmanageable ® airway
obstruction
o Benign ® squamous overgrowth
·
Laryngeal Carcinoma:
o Presentation:
§ Presenting early: if affect vocal chords, invade recurrent pharyngeal
nerve, front of mouth
§ Presenting late: supraglottic lesions due to airway obstruction or pain
(Þ deeper), sinus (lots of space)
§ Dysphagia rare
· 90% are squamous cell carcinoma (like lung)
·
Mostly in males, smoking a major
risk factor, also alcohol, radiation, family history, tend to be older (>
50)
·
Classification, prognosis and
treatment depends on site (prognosis also depends on stage):
o Glottic: 60%, on chords, maintained in larynx by cartilage. Treatment:
radiotherapy unless spread through cartilage
o Supraglottic: 30%, above chords, involves false chord. More aggressive,
metastasise to cervical lymph nodes
o Transglottic: < 5%, crosses from one chord to another
o Infraglottic < 5%, below
chords, more aggressive
·
Don‟t usually metastasise
elsewhere, but lymph node infiltration common
·
Treatment: radiotherapy (® dry
mouth) +/- surgery (superficial, hemilaryngectomy, laryngectomy, laryngectomy
+/- radical neck resection. Chemo has little effect against SCC (most of them).
If laryngectomy then need a tracheostomy (® can‟t cough, infection,
¯humidification, etc)
Lung Cancer
Smoking
·
1998 Statistics for NZ:
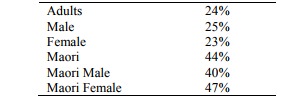
·
Cigarette smoking and lung
cancer:
o Relative risk is 10 times in regular smoker, 20 times in those smoking
> 40 per day
o Most important avoidable cause in 20 – 30% of cancers: including
Respiratory tract, liver, stomach, cervix
o Tobacco and alcohol have a multiplicative relationship in oral cavity,
throat and oesophagus
o Fall in lung cancer mortality begins 5 – 9 years after quitting, back to
baseline at 14 years
o Abnormal cytology and squamous metaplasia in smokers
·
Passive smoking:
o Passive smoking: relative risk is 3 times normal
o Relationship to URTI in children
o Possibility of younger children being affected e.g. SIDS
o Children of smokers more likely to smoke
·
Active Smoking:
o Demonstrates that knowledge/education is insufficient to ensure
behaviour or behaviour change
o Health promotion principles of acting at all levels (i.e.
individual/community/government) to make healthy behaviour the easy choice
·
Measurement: Pack-years =
(cigarettes per day * years smoked) / 20
·
Smoking cessation:
o Listen first: Why do you smoke? (If it‟s stress – what will you do in
the future)
o What do you know about risks (don‟t assume they know about risks – maybe
information lack or cognitive dissonance)
o Estimate cost for them: what would you do with $2-3,000 per year
o Give a positive message: do you want to live longer/better
o Need to negotiate with patient: be smart not paternalistic, be
realistic, honest
o Always put smoking on problem list
o Information: Quit Book or Can Quit (from cancer society). Quitline 0800 778 778
Epidemiology of Lung Cancer
· Commonest cancer in the world
·
In New Zealand, leading cause of
cancer death in men (23%, bowel 15%, prostate 14%) and third most common in
women. Maori women have the highest death rate from lung cancer of any female
population in the world
·
Males predominate. Females catching up
·
60% not resectable at the time of
diagnosis
·
23% of all lung cancers are mixed
·
Smoking:
o > 90% are caused by smoking and are therefore preventable
o 25% of lung cancer in non-smokers is due to passive smoking
·
Types according to smoking
status:
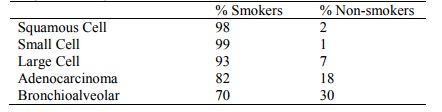
·
Presentation and Survival:
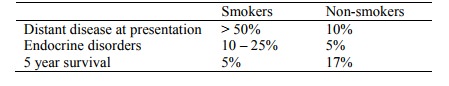
·
Relative incidence changing
rapidly:
o ¯Squamous
cell
o Adenocarcinoma
(now more common than squamous cell in most countries)
o Bronchioalveolar
carcinoma
o Large cell constant
Presentation
·
Fatigue 84%
·
Cough 71%
·
Dyspnoea 59%
·
Anorexia 57%
·
Pain 48%
·
Haemoptysis 25%
Diagnosis
·
Cytology necessary for
management. Use the least invasive route (eg FNA of a neck node if there is
one)
·
Sputum cytology
·
Bronchoscopy:
o Can do washings, brushings, biopsy or lavage (to get more distal stuff)
o If can‟t produce sputum sample, can nebulise with hypo-osmotic saline to
induce sputum
o 1% of transbronchial biopsy ® haemorrhage or pneumonia
·
Fine Needle Aspiration (FNA):
good for peripheral tumours
Types of Lung Cancer
·
Squamous Cell Carcinoma:
o Most common form
o Males > females, with age
o Central tumour: presents late with invasion of lymph nodes
o Can block airway ® distal pneumonia
o Pathogenesis: BPDE in smoke binds p53 mutational hot spots ®
mutation. Sequence of changes from squamous metaplasia to dysplasia to
carcinoma in situ to invasive carcinoma
o Macroscopic: Arises in major bronchus, grey-white hard granular
neoplasm, central cavitation in large cancers, uninvolved lung shows smoking
related pathology (eg emphysema)
o Microscopic appearance: pink when stained (due to cytoplasm), keratin
whirls and intracellular bridges (diagnostic), band in central cytoplasm, large
irregular nucleus, nuclear pleomorphism, hyperchromatism (ie darker), coarse
chromatin clumping, mitosis, large nucleoli, usually arranged in sheets
o Complications: metastatic disease to lymph nodes, brain, liver and
adrenals
o Overall five year survival 10%
o Surgical treatment preferred: but may patients may have insufficient
pulmonary reserve
·
Small Cell Carcinoma:
o = „Oat cell‟ carcinoma
o Central Þ poor prognosis
o Very aggressive
o Treatment: chemotherapy +/- radiotherapy – not surgery as will have
metastasised
o Neuroendocrine origin
o Pathogenesis: BPDE in smoke binds
p53 mutational hot spots ® mutation
o Macroscopic description: perihilar and surround large bronchi. Grey-white
or haemorrhagic. May be more extensive microscopically
o Microscopic appearance: small cells, scant cytoplasm (blue when stained
– predominantly nuclei), ovoid, dense, hyperchromatic so nucleoli not usually
seen, mitotically active, pleomorphic nuclei. Fragile ® crushed
causing blue streaks
o Complications: metastatic disease to lymph nodes, brain, liver and
adrenals
o Two year survival 25%
o Treatment: chemotherapy. Surgery
useless unless palliative
·
Large cell carcinoma:
o Undifferentiated (the „waste basket‟ category)
o Central
o White Þ desmoplastic
o Microscopic appearance: Can‟t tell cell of origin, contains giant cells,
moderate amount of cytoplasm
o Quite aggressive
·
Adenocarcinoma:
o Less common, Male = female
o Occurs peripherally not centrally Þ more easily respectable (unless
into pleura – poor prognosis)
o Less association with smoking
o Association with previous scarring (eg Tb)
o Microscopic appearance: looks like it‟s trying to form glands, ascini,
desmoplastic stroma
·
Bronchioalveolar carcinoma:
o Distinctive variant of adenocarcinoma
o Slowly crawls along bronchioles
o Good 5 year survival but poor prognosis: drown in mucin
o Type of adenocarcinoma
·
Carcinoid tumour:
o Low grade tumour derived from neuroendocrine cells
o Occurs younger (mean is 45) than the more frequent bronchogeneic
carcinomas
o Occur in lung, bowel, other sites
o 90% Central types: 70% survive 5 years
o 10% Peripheral types: rarely metastasise
o Look like oat cell, but behave very differently. Grows by expansion rather than infiltration
·
Mesothelioma:
o Primary pleural tumours, including benign and malignant (also tumours of
the peritoneum, tunica vaginalis and pericardium)
o Benign mesothelioma does not produce pleural effusion and has no
relationship to asbestos
o Malignant mesotheliomas arise in either visceral or parietal pleura, produce pleural effusion (can be unilateral) and are related to asbestos. Drain effusion and re-xray (looking for lumpy pleura). Do cytology on fluid. Invades lung and often other thoracic structures. Presents in 5th to 7th decade, with lag after exposure of > 20 years. Diagnosis by imaging and biopsy. Poor prognosis.
·
Adenosquamous carcinoma: rarer
tumour with squamous and glandular features. Aggressive, bulky, peripheral
tumour
·
Pancoast tumour/syndrome: lung
cancer (usually squamous) in the apex extending to supraclavicular nodes and
involving 8th cervical and 1st and 2nd thoracic nerves ® shoulder pain radiating in ulnar distribution. May also involve
cervical sympathetic nerves and cause Horner‟s Syndrome (ipsilateral
enophthalmos – sunken eye, ptosis, miosis and dry skin)
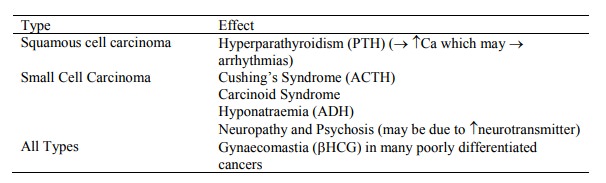
Systemic Effects of Lung Carcinoma
·
Often the presenting problem:
Prognosis
·
No improvement in last 40 years
·
5 year survival for all cases 13%
·
Prognostic factors:
o Stage: most important factor
o Age < 40 worse (diagnosed late)
o Gender: female worse (diagnosed late)
o Site
o Size > 6 cm worse
·
Staging:
o Critical to prognosis and treatment decisions
o Staging systems are regularly refined
o TNM system (not usually used for Small Cell as these have usually
metastasised by diagnosis):
§ T: Size and invasion
§ N: which mediastinal nodes are involved
§ M: no metastases or metastases present
o TNMs are grouped to give stage groups ranging from IA to IV
Treatment
·
Significant difference between
Non-small cell and Small cell:
o Non-small Cell:
§ Resection is the gold standard, but only 20% have resectable disease at
diagnosis. Surgical studies are highly selected and not representative of the
general population
§ Majority will require radiotherapy. Usually palliative, (eg for
haemoptysis, pain or dyspnoea) can also be radical or adjuvant
§ Chemotherapy: not used much in NZ, standard treatment in the US. Cost a
factor in newer agents. Myriad of dosing regimes, combinations, etc. Can be
used prior to surgery/radiotherapy to control micro-metastases/improve
operability, or palliatively. Cisplatin and Etoposide are the gold standards
amongst the older agents
o Small Cell:
§ 70 – 80% have metastasised at diagnosis
§ Very rapid doubling time
§ No place for surgery
§ Mainly managed with chemo +/- radiotherapy (makes a dismal outlook a bit
better)
Related Topics