Chapter: Medicine Study Notes : Respiratory
Adult Pneumonia
Adult Pneumonia
·
= Inflammation and consolidation
of the pulmonary parenchyma
Classifications
·
Community acquired vs. hospital
acquired
·
Typical vs. atypical organisms
·
Lobar vs. diffuse/non-lobar/bronchopneumonia
(although no clinical relevance as it doesn‟t tell you which bug)
·
Normal vs. immunocompromised
·
Severe or not
·
Includes: bronchopneumonia, lobar
pneumonia, interstitial pneumonia, and infectious granulomas
History
·
Previous pneumonia, asthma,
bronchitis
·
Aspiration risk
·
Social History: smoking, alcohol,
occupational or hobby exposure (birds, dust, healthcare worker, etc)
·
Infectious: overseas travel,
recent arrival
·
TB History: race, previous
history, family history, exposure, living situation, BCG status
·
History or immuno-suppression:
transplant, cancer, high dose steroids, HIV risk (sexual, weight loss, night
sweats)
Epidemiology
·
10% of hospitalisations
·
At risk:
o Infants and children: more frequent exposure, immature immune system,
narrower bronchial tree
o Elderly
o Altered level of consciousness: post-operative, CVA, fits,
drugs/alcohol, diabetic coma: diminished cough reflex
o Smokers
o Patients with pulmonary oedema
o Immune deficiencies: leukaemia, lymphoma, renal transplant patients,
cytotoxic drugs
o 80% of AIDs patients die of respiratory failure: 60% of these will have
a pulmonary infection
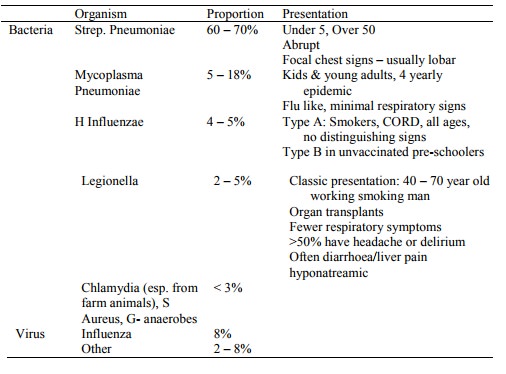
Types of Infectious Pneumonia
Bronchopneumonia
·
Patchy consolidation of the lung.
Infection centered on a bronchus or bronchiole, involving immediately adjacent
alveoli. Pleura not usually involved. Can overlap with lobar pneumonia.
·
Infection is spread through the
airways
·
Macroscopic appearance: patchy
consolidation – firm, raised, nodular, red to grey-white. Colour varies with
the amount of necrosis and haemorrhage, and due to stage. May involve one or
more lobes
·
Microscopic appearance:
o Bronchocentric lesions
o Early: congestion and oedema
o Progresses to: neutrophils + proteinaceous (fibrinous) exudate + RBCs
fill distal airways and alveoli.
o Resolution: airways clear but may organise into fibrous tufts.
Parenchymal destruction depending on organism
·
Causative organisms:
o Depends on whether community or hospital acquired, depressed pulmonary
defences, etc
o G +ive cocci (staphs and streps) and G –ive H Influenza, Pseudomonas, E
Coli and Klebsiella
o S. Aureus and G -ives more common in hospital acquired (eg in ICU) –
also more destructive
o Pseudomonas aeruginosa: can infect lung haematogenously ®
infection of vascular walls ® haemorrhagic pneumonia. Common in burn, immunocompromised and cystic
fibrosis patients. Usually fulminant course
o Legionella pneumonia: characteristic morphology is acute
fibrino-purulent exudative pneumonia – neutrophils + macrophages within a
fibrinous exudate. Inflammatory response spares alveolar
§ walls, so no necrosis or haemorrhage. Mild and self-limiting, except in
elderly and smokers. 10 – 20% mortality in immunocompromised. Rumoured to have
prominent GI symptoms (diarrhoea and vomiting) – but ?any difference in
incidence to other agents. Characteristic in air conditioning (ie plumbers,
office workers, etc) and carriage in potting mix (ie gardeners).
Lobar pneumonia
·
Involves whole lobe uniformly,
often with reactive fibrinous pleuritis
·
95% of cases are Strep pneumoniae
·
Pathogenesis: bacteria inhaled ® profuse
fluid exudate (good growth medium) ® infection spreads through
interalveolar pores throughout lobe
·
Macroscopic and Microscopic
appearance: 4 stages based on macroscopic appearance:
o Congestion: 12 – 24 hours, oedema
o Red hepatisation: 2 – 3 days. Redness due to congestion and haemorrhage.
Fibrinous neutrophilic exudate, consistency of liver
o Grey hepatisation: 3 – 4 days, grey due to WBCs and
fibrin, and ¯blood due to compression of capillaries
o Resolution: 2 – 5 days, macrophage phagocytosis and clearance. Pulmonary
architecture usually maintained, or fibrous tufts fill distal airways and
alveoli and are then incorporated in the interstitium ®
interstitial fibrosis
·
Complications: 20 – 30% get
bacteraemia ® meningitis, endocarditis, arthritis, etc.
·
Presentation: fever, chills,
productive cough with sputum from watery to rusty as the disease advances. ¯Functional
parenchyma ® SOB and cyanotic. Pleural rub.
Lung Abscesses
·
Can occur secondary to pneumonia
or independently. There are two
patterns:
o Multiple abscess: haematogenous spread or bronchopneumonia from a
virulent organism that causes necrosis
o Solitary abscess: usually due to anaerobic organism – eg following
aspiration in alcoholic with depressed reflexes
Infectious Granulomas
·
Three possibilities for a
granuloma:
o Tb: no neutrophil infiltrate in granuloma ®
caseating necrosis
o Fungal: causes abscess Þ neutrophils/puss in the middle
o Sarcoidosis: non-necrotising (non-infectious)
·
Mainly Mycobacterial Tuberculosis:
can infect any organ but commonly the lung
·
Immune cells in granulomas:
o Histiocyte = epithelioid cell = macrophages („eating phase‟ as opposed
to circulating in blood when its called a monocyte)
o Bigger and more cytoplasm than a lymphocyte
o If cytoplasm fuses ® giant cell with multiple nuclei
Tuberculosis
· See also Mycobacteria(Topic)
·
Usually Mycobacterium
Tuberculosis. In AIDS, may be M. avium-intracellulare. M. bovis causes GI Tb in
3rd world from contaminated milk
·
Epidemiology:
o Affects 33% of world‟s population and causes 3 million deaths a year.
o In first world, improved sanitation has reduced incidence – but is
climbing again due to AIDS and antibiotic resistance
o NZ: 300 notifications per year: European < Maori < PI < Other
·
Clinical:
o Non-specific fever and weight loss (due to macrophage cytokines),
coughing, blood-tinged sputum. If in GI, can present with obstruction
o Takes 6 weeks to 3 months before Tb sensitivity develops (ie Mantoux
positive)
o Predisposing host factors: malnutrition, alcohol, diabetes, age, immune
suppression (diseases or drugs), background population prevalence
·
Progression:
o Primary infection: initial exposure is self-limiting, leading to
formation of a solitary granuloma (Ghon focus), often with granulomas along
lymphatic drainage and in hilar lymph nodes (Ghon Complex). Lesions usually
asymptomatic and undergo fibrosis and calcification
o Spontaneous recovery: may still have bacilli on board
o Progressive primary infection: rare, primary lesion erodes into airways
or vasculature ® airway spread or miliary spread ® fulminant bronchopneumonia
o Post-primary pulmonary Tb: granulomas coalesce ®
consolidation evident on X-ray ® cavity ruptures into a bronchus ® productive cough, fever,
sweating, haemoptasis
o Secondary infection: in small percentage of those who had primary
infection. Reactivation of latent mycobacteria. Usually in lung apices (higher
O2 tension). Can become progressive. Can have isolated involvement of the
intestine or adrenals (® acute Addison‟s Disease). Cell mediated immunity or delayed type
hypersensitivity contributes to tissue destruction
·
Diagnosis:
o Samples: sputum, bronchial wash, gastric lavage in the morning,
bronchoscopy, pleural tap
o Culture (6 weeks), ZN stain, PCR (not very sensitive or specific for
serious disease)
·
Treatment:
o Combinations always required for a long duration
o Drugs:
§ Isoniazid: best and cheapest. Bacteriocidal. Side effects: rash, peripheral neuropathy, hepatotoxicity
§ Rifampicin: Destroys rapidly dividing bacilli quickly (Þ good for
fulminant disease). SE: enzyme induction,
orange secretions, rash, flu like illness, purpura
§ Pyrazinamide: bacteriocidal, works intra-cellularly (ie bacilli inside
macrophages). SE rash, hepatotoxicity, gout
§ Ethambutol: SE optic neuritis. In kids too young to monitor visual acuity,
use streptomycin
o Regime: 2 months of isoniazid + rifampicin + pyrazinamide + 4 months of
just isoniazid and rifampicin
o Compliance a major issue (® directly observed therapy. Is
cost effective compared to self-administered therapy. Treatment completion
rates up to 90% are possible), also toxicity
o May need steroids (in addition to antibiotics) if adrenal suppression,
miliary Tb or pleural effusion
·
Pathology:
o Bacterium is ingested by macrophages, but resists lysis due to waxy
coat. Multiplies inside macrophage. Immune response forms granuloma through
unknown mechanisms
o Macroscopic appearance: lesions in any organ – but mainly in lungs and
lymph nodes. Initially small focus of consolidation < 3cm with central
caseation, which cavitates if it communicates with a bronchiole. Resolution ®
fibrocalcific scarring puckering the pleural surface. Large nodules have
extensive cavitation and necrosis, and are lined with a ragged white material
containing millions of mycobacteria
o Microscopic appearance: granulomas composed of epitheliod cells
surrounded by fibroblasts and lymphocytes, containing giant cells and Langhans
cells (nuclei around the edge). Central caseous necrosis. Acid-fast bacilli
with ZN stain
Fungal Pneumonias
·
Second most common cause of
infectious granulomas
·
Often form necrotising granulomas
with central cavitation similar to Tb
·
Uncommon in NZ: but query in
returned travellers or immunosuppressed
·
Causative agents:
o Candida: includes yeast and pseudohyphae. Oral commensal ® multiple
scattered lesion in the lung
o Aspergillus: a saprophytic hyaline mould causing bronchopneumonia, possibly with vascular invasion and dissemination ® haemorrhage and necrosis. Most common in immunocompromise – especially acute leukaemia
o Mucormycosis (Zygomycosis): 2 infectious types: Rhizopus and Mucor.
Tendency to invade blood vessels and cause haemorrhagic pneumonia
o Cryptococcus neoformans: pleomorphic round to oval 4 – 10 micron yeast
with thick mucinous capsule. Found in bird (pigeon) droppings. Most common
infection is meningitis. Stains with Indian Ink stain
o Others: histoplasma capsulatum, coccidioides immitis and blastomycosis
dermatitidis
Viral pneumonias
·
Usually acquired through
inhalation
·
Typically result in diffuse
interstitial oedema and lypmhocytic cellular infiltrates in the septae. Lungs
tend to be heavy and diffusely firm without focal lesions. If severe ®
microvascular injury ® pneumocyte necrosis and leakage of proteinaceous fluid into alveoli ® hyaline
membrane formation
·
Most due to influenza viruses
(elderly), respiratory syncytial virus (kids) and rhinovirus (kids)
·
Viruses of note:
o Cytomegalovirus: Herpes virus causing cytomegaly or enlargement of
infected cells. May have multiple small cytoplasmic inclusions that are purple
and PAS-positive. Subclinical infection unless immunocompromised. Commonest
viral pneumonia in immunosuppressed. Focal or diffuse interstitial pneumonia.
CMV primary infects epithelial and endothelial cells
o Herpes Simplex Virus types I and II. Have characteristic nuclear
inclusions in epithelial cells. Two patterns of spread: Necrotising
Tracheobronchitis mechanism (spread by contiguity through necrotic mucosa) or
Haematogenous dissemination (more random distribution through lung)
o Varicella Zoster: Lung involvement similar to H. Simplex
o Measles: RNA virus, infection leads to multinucleate giant cells,
interstitial pneumonia, and focal bronchilobar necrosis. Mainly in immunocompromised
kids with measles
o Adenovirus: DNA virus mainly causing mild upper RTI. Clinical disease in
transplant patients (eg bone marrow). Necrotising bronchitis and bronchiolitis.
Smudge cells seen (large cells with dense mass filling the nucleus)
o Influenza: RNA virus seen in older adults
o Respiratory Syncytial Virus: RNA virus causing RTI in the young. Causes
bronchiolitis, sometimes necrotising, and less frequently interstitial
pneumonia
·
Mainly Influenza A or B,
Adenovirus or RSV
Other pneumonias
·
Mycoplasma pneumonia: Common
cause of URTI. Smallest free-living organism. 15% of all pneumonias in general
population. Benign and self-limiting with few complications. Peak incidence is
5 – 15 years. Causes a bronchiolar lesion with neutrophil rich exudate, and
bronchiolar metaplasia
·
Pneumocystis Carinii Pneumonia:
Extracellular protozoan parasite almost exclusively infects the lung. Selective
attachment to type I pneumocytes ® injury. Usually in AIDs.
Microscopic appearance: interstitial infiltrate of lymphocytes and plasma
cells, and foamy intra-alveolar exudate containing the organism. Stain with
silver (GMS). Occurs as cysts, excysted forms and trophozoites. Ground glass
appearance on X-ray
·
Lipid Pneumonia: Exogenous lipid
pneumonia – aspirated mineral oil being taken by the elderly for constipation ®
segmental opacification (whiting-out) of the lung and granulomatous fibrous
reaction. Endogenous lipid pneumonia occurs distal to an obstruction (eg
cancer) due to coalescing lipid droplets from dead alveolar macrophages
·
Mixed bacterial flora is normally
found in patients with chronic pulmonary infections (eg cystic fibrosis,
bronchiectasis). Principle organisms are Pseudomonas Aeruginosa (commonest),
staphylococcus aureus and Haemophilus influenzae
Community Acquired Pneumonia
Epidemiology
·
1 per 1,000 admitted annually
·
Mortality = 10 % (especially old,
young, underlying disease)
Pathogens:
·
Unknown organism in 1/3 of cases
despite extensive testing. Dual
infections occur
·
GI symptoms in typical and
atypical
·
Clinical clues:
o 2 – 3 days: pneumococcus, staph aureus
o 1 – 3 weeks: mycoplasma/legionella
o Sputum: foul smelling Þ anaerobic, rust coloured Þ pneumococcal
o Season: summer Þ legionella, mycoplasma comes in 4 yearly cycles
o Chronic lung disease: H Influenzae, Moraxella catarrhalis (ie b lactams)
o HIV: PCP
o Neutropenia: G –ive, fungal
o Alcohol: G –ive, legionella, staph
·
Aspiration (6 – 10%) ® risk of
anaerobe ® cavitation. Upper respiratory
commensals
·
Cavitation ® S
Aureus, G- & Tb
·
Previous viral infection common
in bacteria
·
If immunocompromised:
o Pneumocystis carinii (AIDs)
o G – ive bacilli: pseudomonas aeruginosa, Klebsiella pneumoniae
(neutropenic cancer patients)
o Fungi: Candida albicans, Cryptococcus neoformans
o Virus: cytomegalovirus
Diagnosis
·
Suggested by fever + respiratory
symptoms (cough, sputum, dyspnoea)
·
May present with GI symptoms most
prominent
·
Confused with acute bronchitis
·
Signs: fever in > 80%,
Respiratory Rate > 20, crackles on auscultation, consolidation in 30%
·
Post influenza: 70% (?) S. Aureus
infection (® micro abscesses)
·
Can be secondary to abscess,
empyema, lung cancer
Investigation Options
·
CXR: extent, cavitation,
effusion, cardiomegaly. False negatives possible if PCP or during first 24
hours
·
Blood gases
· FBC: White cell count, if > 15,000 * 10E9 Þ bacteria likely cf. virus
·
Urea/electrolytes/liver ® severity
and underlying disease
·
Urine: glycosuria
· Microbiology:
o Sputum (but 1/3 don‟t expectorate and many causative organisms are URT
commensals): culture and pneumococcal antigen test (most sensitive test for
strep pneumoniae). If can‟t get sputum sample, can nebulise with hypo-osmotic
saline.
o Blood serum for pneumococcal antigen
o Blood cultures
o Culture plural effusion
·
Lavage via bronchoscopy may be
indicated in immunosuppressed patients and in those suspected of TB who can‟t
produce adequate sputum
·
Acute and convalescent serum for
antibodies to mycoplasma pneumoniae, legionella, chlamydia pneumoniae
(Convalescent = 5 – 6 weeks later, a 4 fold rise in antibody titre or the
presence of IgM specific antibody is evidence of recent infection)
Prognosis
·
Classified as severe if (21 times
risk of mortality)
o Age > 65
o Respiratory rate > 30 bpm. (key prognostic indicator)
o Systolic BP < 90, Diastolic BP < 60 mmHg or low urine output (ie
shocked)
o Confusion
o Serum urea > 7 mmol/L
o Comorbid disease: heart failure, diabetes, CORD, cancer, HIV, renal
failure, chronic alcohol, etc
·
Other markers of severe
prognosis:
o WBC < 4000 or > 30000
o PO2 < 60 or inability to get Sats above 90% despite O2
therapy
o CXR shows multilobed or pleural effusion
o Haematocrit < 30%
Treatment
·
Community treatment:
o Immediate empirical therapy:
§ Should cover S pneumonia
§ Erythromycin if legionella/Mycoplasma suspected
o Antibiotics: for 5 – 10 days (10 – 14 if Mycoplasma or Chlamydia)
§ Oral amoxycillin 500mg td
§ If allergic to penicillin: erythromycin
§ IV benzyl penicillin 1.2 g qd IV if poor absorption (e.g. vomiting)
§ If severe: erythromycin 1g qd + 3rd generation cephalosporin
o Types of antibiotics:
§ Penicillin: strep pneumoniae. Even if resistant, iv penicillin dose exceeds the MIC, so it‟s still effective (doesn‟t work though for Meningitis caused by Strep Pneumoniae because CSF penetration is lower)
§ Augmentin, Cefaclor, Tetracycline (not kids), cefuroxime (iv): H
Influenzae (5% resistant to amoxycillin), Branhamella Catarrhalis
§ Flucloxacillin: Staph aureus
§ Ceftriaxone: penicillin resistant strep pneumoniae, G- bacilli
§ Erythromycin (ie macrolides): mycoplasma, legionella, chlamydia
§ Rifampicin + isoniazid + pyrazinamide: Tb
§ Cotrimoxazole: Pneumocystis carinii
§ Fluconazole or Amphotericin B: Candida, Cryptococcus
§ Ganciclovir: CMV
o Resistant to Augmentin (ie have b-lactamase):
§ Mycoplasma pneumoniae
§ Chlamydia pneumoniae
§ Legionella
§ Penicillin resistant strep pneumoniae
·
Hospital treatment:
o Only 0.1% of chest infections get to hospital Þ not
typical of population as a whole
o Hospitalise if high pyrexia, cyanosis, tachycardia, tachypnoea,
confusion
o Oxygen:
§ See Oxygen Therapy(Topic)
§ Give sufficient O2 to keep PO2 > 60 mmHg
§ O2 saturation > 90 % preferable
o Transfer to ICU if:
§ Severe
§ Blood gases bad: PO2 < 60 on FIO2 > 60%, or PCO2 > 48 (should breath faster ® PCO2 should fall – if normal or raised person getting tired ® bad sign)
§ Shocked
·
CCHL preferred medicines list:
o Uncomplicated: Penicillin G 1.2 g iv 4 – 6 hourly or amoxycillin 1g iv 8
hourly. Consider adding erythromycin 500 mg iv 6 hourly if the patient is >
60, no response to penicillin antibiotics, or mycoplasma or legionella are
suspected (atypicals less likely if leucocytosis)
o History of CORD or other disease: Augmentin 1.2 g iv 8 hourly or
Ceftriaxone 1.5 g iv 8 hourly. Consider adding erythromycin for above
complications
Failure to Respond
·
Is treatment failing?
o Some improvement should be seen in 48 – 72 hours, don‟t change treatment
over this time unless there is a marked deterioration
o CXR may worsen initially after therapy started: if mild pneumonia this
may be normal. If severe, this is a poor prognostic indicator
o Fever lasts 2 – 4 days, S pneumoniae resolves quickest
o Crackles will last beyond 7 days in up to 40%. May take more than a month for CXR to clear
·
If treatment is failing,
consider:
o Incorrect diagnosis: PE, pulmonary oedema, Wegerner‟s granulomatosis (ie
non-infectious illness)
o Antibiotic resistant organism
o Resistant infection: mycoplasma, chlamydia, Staph aureus, TB, PCP
(immunodeficient)
o Complication: empyema (see Pleural Disease), abscess, PE, drug induced fever
o Underlying disease: lung cause, cardiac failure, immunodeficiency
o Drug compliance in outpatients
Related Topics